

Original Article - Year 2012 - Volume 27 -
Lipoabdominoplasty in the aesthetic treatment of the abdomen: 5 years of experience
Lipoabdominoplastia no tratamento estético do abdome: experiência de 5 anos
ABSTRACT
BACKGROUND: Abdominoplasty aims to reduce saggy skin and excessive skin and adipose tissue, as well as to improve curves, the shape of the waist, and the volume of the abdomen. In order to enhance aesthetic results, additional operative techniques such as liposuction are associated with abdominoplasty. This study aims to demonstrate the surgical technique of lipoabdominoplasty used by the senior author during a period of 5 years, and evaluate the results and complications in patients with indication for classic abdominoplasty.
METHODS: We performed a retrospective study using medical records from a group of 162 patients who underwent lipoabdominoplasty associated with other procedures or not, from May 2006 to May 2011. The age of the patients ranged from 33 to 62 years.
RESULTS: In all cases, we achieved significant reduction of skin and adipose tissue, together with a decrease in amount of saggy skin and improvement in body shape. The incidence of postoperative complications such as necrosis, irregularities in the infraumbilical adipose tissue, seromas, hematomas, epidermolysis, and dehiscence in this study was low, similar to the literature findings.
CONCLUSIONS: Lipoabdominoplasty is a safe procedure, and has low complication rates when the safety criteria that permit a wellvascularized flap with preservation of the perforant arteries are followed. Association of lipoabdominoplasty with liposuction in the abdominal area and body shaping is considered safe and essential when seeking better body harmonization and aesthetic results, which results in improved patient satisfaction.
Keywords: Abdomen/surgery. Lipectomy. Plastic surgery. Abdominal wall.
RESUMO
INTRODUÇÃO: Na abdominoplastia, busca-se reduzir a flacidez e o excesso cutâneo-adiposo, melhorando curvas, cintura e relevo do abdome. Na busca por resultados estéticos mais satisfatórios, técnicas operatórias são associadas, como a lipoaspiração, na tentativa de atingir esses resultados. Este estudo teve por objetivo demonstrar a técnica cirúrgica de lipoabdominoplastia adotada pelo autor sênior ao longo de cinco anos e avaliar resultados e complicações em pacientes com indicação de abdominoplastia clássica.
MÉTODO: Foi realizado estudo retrospectivo, por meio da revisão de prontuários, de um grupo de 162 pacientes submetidas a lipoabdominoplastia associada ou não a outros procedimentos, no período de maio de 2006 a maio de 2011, no Núcleo Hermínio Amorim - Cirurgia Plástica e Tratamentos Estéticos (Lavras, SP, Brasil). A idade das pacientes variou entre 33 anos e 62 anos.
RESULTADOS: Em todos os casos foi observada redução significativa do tecido cutâneo-adiposo, com expressiva diminuição da flacidez abdominal e melhora do contorno corporal. A incidência de complicações pós-operatórias, como necroses, irregularidades do tecido adiposo infraumbilical, seromas, hematomas, epidermólises e deiscências, encontrada neste estudo é baixa e está de acordo com a literatura.
CONCLUSÕES: A técnica de lipoabdominoplastia é um procedimento seguro, com baixo índice de complicações, desde que respeitados os critérios de segurança, que permite a obtenção de retalho bem vascularizado, com preservação das artérias perfurantes. A associação da técnica de lipoaspiração realizada no abdome e no contorno corporal é considerada segura e essencial na busca por melhor harmonia corporal, por melhores resultados estéticos e, consequentemente, por maior satisfação do paciente.
Palavras-chave: Abdome/cirurgia. Lipectomia. Cirurgia plástica. Parede abdominal.
Abdominal dermolipectomy has been performed for more than a century. In 1899, Kelly was the first author to use the expression abdominal lipectomy1. Schulta published 2 cases of transversal abdominal dermolipectomy in 19081. In 1939 and 1942, Thorek reported performing an abdominal dermolipectomy surrounding the trunk and subcostal inverted abdominal dermolipectomy to correct a "bat wing" deformity1. In 1943, Prudente referred to the importance of preserving the umbilicus1. In 1963, Callia reported the resulting scar over the pubis, with low lateral extensions, parallel to the inguinal folds, and described technical aspects related to removing and re-inserting the umbilicus1. Pitanguy defended strengthening of the musculoaponeurotic system through horizontal folding of the sleeves of the rectus abdominus muscles in the middle line in 19671. Pontes, in 1964, and Serson, in 1969, reported an abdominoplasty technique with previous incision of the excessive skin and adipose tissue1. In 1972, Rebello1 described inverted abdominal dermolipectomy with incision in the submammary creases. Sinder published a technique of transversal abdominal dermolipectomy in 1975, demonstrating excision of the excessive skin and adipose tissue after traction1. In 1976, Avelar2 proposed a 3-point star-shaped incision to transpose the umbilicus. Hakme3 reported performing longitudinal peri-and supraumbilical lipectomy in 1979. In 1998, Baroudi & Ferreira4 contributed significantly to abdominoplasty by publishing a paper about prophylaxis for and treatment of seroma. Jaimovich et al.5 described the importance of abdomen semiology in the planning of abdominoplasty in 1999.
In conclusion, the evolution of techniques has resulted in abdominoplasty becoming a more elaborate surgery, enabling surgeons to obtain good results. By popularizing the liposuction technique, Illouz6 was most responsible for the beginnings of plastic surgery. After this, several other publications concerning the classification and treatment of abdominoplasty associated with liposuction emerged7,8, including superficial liposuction9 and the new technique of abdominoplasty with a closed vascular system2. These and several other important publications were essential for the advancement of liposuction associated with abdominoplasty. Saldanha et al.10 proposed a technique of lipoabdominoplasty with selective detachment, which represented a significant contribution to the evolution of liposuction associated with abdominal plastic surgery.
This study aims to demonstrate the surgical technique of lipoabdominoplasty adopted by the senior author during a period of 5 years and evaluate results and complications in patients indicated for classic abdominoplasty.
METHOD
A retrospective study was performed by reviewing the medical records from a group of 162 patients who underwent lipoabdominoplasty from May 2006 to May 2011 at Núcleo Hermínio Amorim de Cirurgia Plástica e Tratamentos Estéticos (Herminio Amorim Center of Plastic Surgery and Aesthetic Treatments, Lavras, SP, Brazil). Lipoabdominoplasty alone was performed in 114 patients, while 48 patients underwent other associated procedures.
Preoperative evaluations included laboratory examinations, cardiology and anesthesiology tests, and examination of photographic records. Patients were aged between 33 and 62 years, and their body mass index ranged from 25 kg/m2 to 32 kg/m2. All patients had a type V abdomen, according to the classification of Jaimovich et al.5.
Surgical markings were made twice. First, with the patient in standing position (Figure 1), the middle line of the abdomen and the horizontal lower suprapubic line (around 12 cm long) were marked using a surgical pen, at the height of the pubic hair or over the cesarean scar, when existent. The markings were extended from the horizontal line to the lateral lines of the hip, measuring generally 12-14 cm, following the abdominal crease; an upper line shaped like a spindle, hollow below, was passed next to the upper part of the umbilical scar and inferiorly lengthened until the lateral part of the horizontal line of the abdomen.
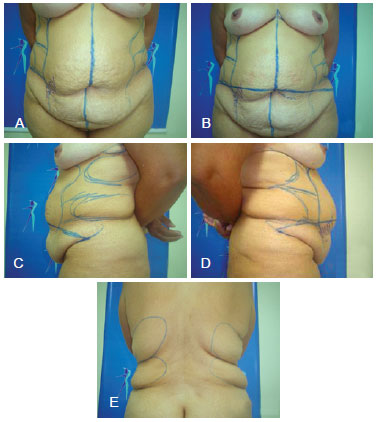
Figure 1 - Surgical markings with the patient standing upright. In A and B, anterior view. In C, left side. In D, right side. In E, posterior view.
The areas where liposuction was to be performed were marked with curved and circular lines. Subsequently, with the patient in a supine position in the operating room, the second set of the surgical markings was made (Figure 2). The markings made in the upright position were revised using a ruler, with the aim of achieving symmetry and a suitable scar. The suprapubic scar was localized about 7-cm above the vaginal fork.

Figure 2 - Markings in the supine position.
Surgeries were routinely performed under epidural block and sedation, with the supervision of an anesthesiologist, antibiotic prophylaxis, and antithrombotic prophylaxis with low molecular weight heparin, when indicated, in accordance with the prevention protocol used by Ivo Pitanguy Clinic11. Compressive stockings and veno-compressors were used in the lower limbs.
The surgical procedure started with infiltration of the entire previously marked abdominal region with 500 mL of 0.9% saline solution and 1/500,000 IU epinephrine. Deep liposuction was performed in the upper abdomen (Figure 3) and flanks, followed by superficial and deep liposuction of the lower abdomen using 4-mm and 5-mm tubing.

Figure 3 - Liposuction of the upper abdomen.
Once liposuction was concluded, an incision was made around the umbilicus and the area of the flap to be removed using a high frequency scalpel, surrounding the umbilicus by about 2.5 cm (Figure 4). The flap was lifted from the lateral parts, preserving the scarpa fascia, and removed as a single piece (Figure 5). Cauterization followed routine procedures, starting with supraumbilical detachment and along the middle part of the rectus abdominus muscles (Figure 6). In the infraumbilical region, one central rectangular segment of adipose tissue was removed to identify the borders of the rectus abdominus muscles (Figure 7). Another cauterization was carried out, followed by correction of diastasis of the rectus abdominus muscles by plicating the anterior rectus sheath 1 cm from the medial margin of the muscle in a single xifopubic plane12 by using separated and inverted "X" sutures. At the same time, fixation and shortening of the umbilical pedunculus were carried out close to the abdominal aponeurosis by means of a suture in the upper and lower parts13 (Figure 8).
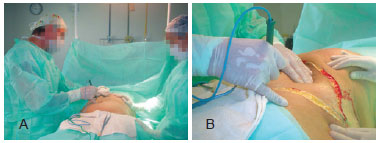
Figure 4 - In A, incision in the flap area. In B, incision of the umbilicus area.
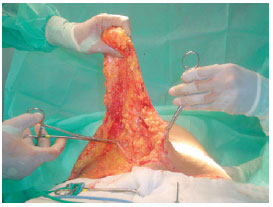
Figure 5 - Removal of the flap.

Figure 6 - Supraumbilical detachment.

Figure 7 - Removal of the infraumbilical subcutaneous tissue.
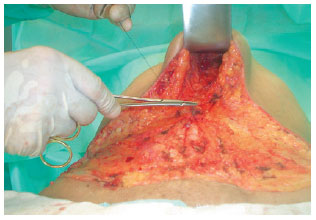
Figure 8 - Plicature of the rectus abdominus muscles and fixation and shortening of the umbilical pedunculus.
Once the plicature of the rectus abdominus muscles was finalized, the dorsal part of the table was elevated and previous closure of the upper flap was performed using 2 sutures in the lower line of the upper margin of the flap with the middle line of the suprapubic region. The projection point for transposition of the umbilicus in the middle line was marked using long Allis tweezers, also orienting through the height of the plane of the antero-superior iliac spine. We then made a 1.5-cm long horizontal incision, which was arched slightly upwards, using the high frequency scalpel (Figure 9), removed the closure points, and elevated the flap to perform a periumbilical lipectomy.

Figure 9 - Skin incision to transpose the umbilicus.
After revising the abdominal wall, we initiated closure by fixing the upper flap to the abdominal aponeurosis using Baroudi sutures4. Next, transposition of the umbilicus through single separate sutures directly on the skin was performed (Figure 10). The Baroudi4 sutures were passed in the flanks and infraumbilical regions. Closure of the upper abdominal flap with sutures in 3 planes was carried out, with a continuous aspiration drain inserted at the time of suture.
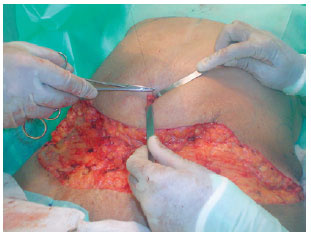
Figure 10 - Transposition and fixation of the umbilicus.
Finally, the surgical incision was revised (Figure 11) and the wound was treated. Patients were dressed in a girdle and assisted to their beds in the ward after clearance by the anesthesiologist.

Figure 11 - Closure of the upper abdominal flap.
Patients were discharged the day after surgery, after clinical evaluation, re-dressing of the wound, and evaluation of the scar and operated area, as well as removal of the drain. Patients received written instructions and analgesics, anti-inflammatory drugs, and low molecular weight heparin were prescribed when indicated, according to protocol. They were instructed to walk shortly after surgery, while keeping their upper body bent low, and to rest in the Fowler position for 7 days. Postoperative physiotherapy was initiated within 72 to 96 h. The girdle was maintained for 60 to 90 days.
Follow-up appointments to evaluate progress were conducted weekly in the first postoperative month and monthly until the third month, with the last appointment at 6 months, after which the results were evaluated.
RESULTS
In all cases, we obtained significant reduction of the skin and adipose tissue, with decreased saggy abdominal skin and improvement of the body contour, as well as better positioning of the margins of the upper flap in the inguinal and pubic region, without un-leveling or adipose "step."
There were no deaths, or cases of deep vein thrombosis, emboli, or infection. However, the following complications were observed: 1.8% of cases developed necrosis in the infraumbilical and suprapubic region; 2.5% of cases showed irregularity of the subcutaneous tissue; 2.5% of cases developed epidermolysis; 3.7% developed hematoma, 4.9% showed scar dehiscence; 9.3% developed seroma; and 19.1% showed a hypertrophic scar, 7.5% of which occurred in the umbilical region and 11.6% in the umbilical and suprapubic regions (Figure 12).
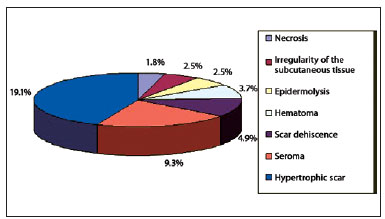
Figure 12 - Postoperative complications.
Cases of necrosis were followed up during a period of 4-5 months, with debridement and closure of the borders and completion with sutures in 3 planes. This resulted in enlarged scars of 2-5 cm that the patients did not wish to correct.
Cases of superficial epidermolysis showed a good evolution, with spontaneous resolution. Patients with subcutaneous irregularities needed surgical revision with liposuction under local anesthesia. Suctioning of 40-60 mL of fat by using a 20 mL syringe and 2 mm tubing resulted in good evolution.
Hematomas were observed at the 1-week follow-up and were treated with aspiration puncture by using a 40 mm × 12 mm needle. Drainage of 30 mL to 60 mL of fluid resulted in good evolution. Cases of seroma were identified at the 2-week follow-up; 12 of these cases had a clinical diagnosis and another was detected by Doppler ultrasonography. These 13 patients were treated using sequential aspiration puncture with a 40 mm × 12 mm needle. Aspiration of 40 mL to 120 mL of fluid resulted in resolution within 4 weeks. Two cases of seroma showed spontaneous drainage through the scar, and resolved within 6 weeks postoperatively.
Scar dehiscence occurred in the suprapubic region, with a length of about 3 to 5 cm. Drainage of the sero-hematoma was found without signs of infection, and the patients were treated with surgical revision and new sutures in 3 planes under local anesthesia, which resulted in good scar evolution.
Concerning the evolution of hypertrophic scars, only 9 patients to date have accepted surgical correction, which produced a good final result.
DISCUSSION
Loss of body harmony, usually caused by post-pregnancy changes, excess body weight, or ageing is a major reason for displeasure leading to abdominal plastic surgery. Abdominoplasty aims to reduce saggy skin and excessive skin and adipose tissue, as well as to improve curves, the shape of the waist, and the size of the abdomen. To produce better aesthetic results, other operative techniques such as liposuction are often associated with abdominoplasty.
Successful lipoabdominoplasty hinges on diminished detachment of the abdominal flap3; the improved viability and safety of a less detached flap with preserved vascular and sensitivity sources cannot be denied. The improved safety resulting from better flap vascularization has been described in Doppler studies14 and is confirmed by the eco-Doppler examination performed in one of our patients on the 19th postoperative day after lipoabdominoplasty, which confirmed preservation of the perforant arteries.
The possibility of improved body shape and enhanced thickness of the abdominal wall is another important characteristic of this technique. This provides refinement and better suitability of the upper flap to the suprapubic and inguinal area, as already described by several authors2,3,7,8, and allows a more harmonious result with better shape and tissue accommodation (Figures 13 to 18).

Figure 13 - A patient who underwent lipoabdominoplasty for aesthetic treatment of the abdomen. In A, C, and E, preoperative appearance in anterior, right, and left views, respectively. In B, D, and F, postoperative appearance in anterior, right, and left views, respectively.

Figure 14 - A patient who underwent lipoabdominoplasty for aesthetic treatment of the abdomen. In A, C, and E, preoperative appearance in anterior, right, and left views, respectively. In B, D, and F, postoperative appearance in anterior, right, and left views, respectively.
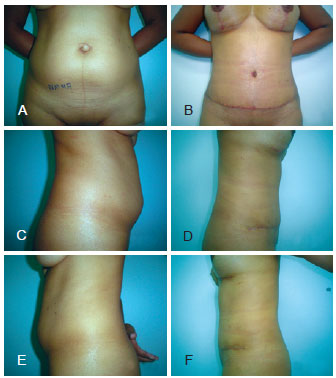
Figure 15 - A patient who underwent lipoabdominoplasty for aesthetic treatment of the abdomen. In A, C, and E, preoperative appearance in anterior, right, and left views, respectively. In B, D, and F, postoperative appearance in anterior, right, and left views, respectively.
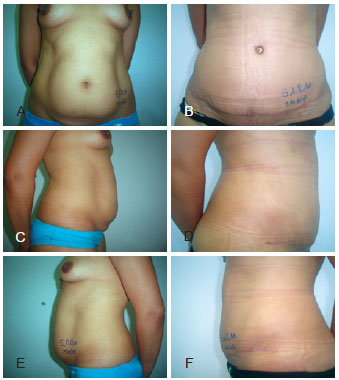
Figure 16 - A patient who underwent lipoabdominoplasty for aesthetic treatment of the abdomen. In A, C, and E, preoperative appearance in anterior, right, and left views, respectively. In B, D, and F, postoperative appearance in anterior, right, and left views, respectively.
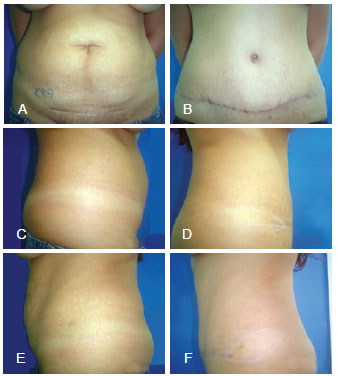
Figure 17 - A patient who underwent lipoabdominoplasty for aesthetic treatment of the abdomen. In A, C, and E, preoperative appearance in anterior, right, and left views, respectively. In B, D, and F, postoperative appearance in anterior, right, and left views, respectively.
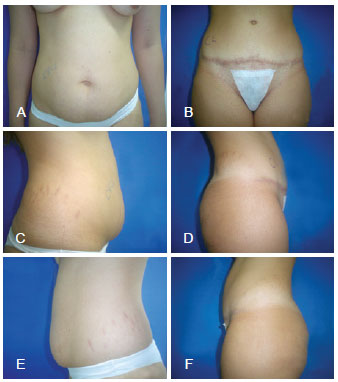
Figure 18 - A patient who underwent lipoabdominoplasty for aesthetic treatment of the abdomen. In A, C, and E, preoperative appearance in anterior, right, and left views, respectively. In B, D, and F, postoperative appearance in anterior, right, and left views, respectively.
The learning curve for this technique is not easy and it, like any other surgery, demands good anatomical knowledge and respect for the limitations of the abdominoplasty technique with regards to detachment and reduction of the thickness of the subcutaneous layer of the abdominal wall according to the liposuction technique3. The removal of the tissue in one single block, before detaching the upper abdomen1, decreases the surgical time. This is an important factor in preventing postoperative complications and is essential for the best postoperative recovery and aesthetic results.
Plicature of the rectus abdominus muscles, first described by Pitanguy, is essential for contention, reinforcement, and modeling of the volume of the abdomen.
The quality of the scars and the shape of the umbilicus deserve to be highlighted, since they are often the first aspects of the abdomen to be evaluated. As a consequence of its central position in the abdomen, the umbilicus is frequently observed and analyzed, and is therefore crucial for good aesthetic results. There are several techniques for repairing the umbilicus and periumbilical refinement12.
The incidence of postoperative complications such as necrosis, irregularities of the infraumbilical adipose tissue, seromas, hematomas, epidermolysis, and dehiscence found in this study follows the trends found in the literature4,15-17. Scar alterations show a higher incidence compared to other complications, which deserves further evaluation. However, this does not constitute a limiting factor for the indication of this lipoabdominoplasty technique. Patients must be informed about the possibility of the occurrence of each complication, as well as the possible need for surgical revision of the scar in the late postoperative period (Figure 19).
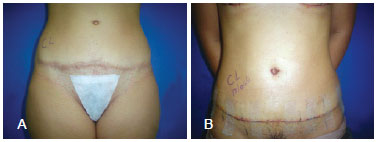
Figure 19 - In A, preoperative appearance before scar correction. In B, postoperative appearance.
CONCLUSIONS
The lipoabdominoplasty technique is a safe procedure with low complication rates, as long as the safety criteria allowing a well-vascularized flap and preservation of the perforant arteries are respected. The association of liposuction with abdominal reshaping is considered safe and essential to ensure better body harmony, aesthetic results, and patient satisfaction.
REFERENCES
1. Sinder R. Cirurgia plástica: abdominoplastia. São Paulo:Atheneu; 2005. p. 621-45.
2. Avelar JM. Uma nova técnica de abdominoplastia: sistema vascular fechado de retalho subdérmico dobrado sobre si mesmo combinado com lipoaspiração. Rev Bras Cir. 1999;88/89(1/6):3-20.
3. Hakme F. Lipectomia peri e supra-umbilical nas abdominoplastias. Rev Bras Cir. 1979;69:271.
4. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
5. Jaimovich CA, Mazzarone F, Parra JFN, Pitanguy I. Semiologia da parede abdominal: seu valor no planejamento das abdominoplastias. Rev Soc Bras Cir Plást. 1999;14(3):21-50.
6. Illouz IG. Une nouvelle technique pour les lipodystrophies localisées. Rev Chir Esth Franc. 1980;6:10-2.
7. Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg. 1991;15(2):111-21.
8. Swift RW, Matarasso A, Rankin M. Abdominoplasty and abdominal contour surgery: a national plastic surgery survey. Plast Reconstr Surg. 2007;119(1):426-7.
9. Souza Pinto E. Lipoaspiração superficial. Rio de Janeiro: Revinter; 1999. p. 59-92.
10. Saldanha OR, Pinto EB, Matos WN Jr, Lucon RL, Magalhães F, Bello EM. Lipoabdominoplasty with selective and safe undermining. Aesth Plast Surg. 2003;27(4):322-7.
11. Paiva RA, Pitanguy I, Amorim NFG, Berger R, Shdick HA, HolandaTA. Tromboembolismo venoso em cirurgia plástica: protocolo de prevenção na Clínica Ivo Pitanguy. Rev Soc Bras Cir Plást. 2010;25(4):583-8.
12. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg. 2001;108(6):1787-95.
13. Mello DF, Yoshino H. Plicatura da base umbilical: proposta técnica para tratar protrusões e evitar estigmas pós-abdominoplastia. Rev Bras Cir Plást. 2009;24(4):525-9.
14. Graf R, Freitas R, Fisher M, Bark A, Loureiro A, Pianowski R, et al. Estudos de fluxometria Doppler. In: Saldanha OR, ed. Lipoabdominoplastia. Rio de Janeiro: Di Livros; 2004. p. 87-92.
15. Ferreira MC. Cirurgia plástica estética: avaliação de resultados. Rev Soc Bras Cir Plást. 2000;15(1):55-61.
16. Martino MD, Nahas FX, Novo NF, Kimura AK, Ferreira LM. Seroma em lipoabdominoplastia e abdominoplastia: estudo ultra-sonográfico comparativo. Rev Soc Bras Cir Plást. 2010;25(4):679-87.
17. Dillerud E.Abdominoplasty combined with suction lipoplasty: a study of complication, revisions, and risk factors in 487 cases. Ann Plast Surg. 1990;25(5):333-8.
1. Full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP; owner and director of Núcleo Hermínio Amorim de Cirurgia Plástica e Tratamentos Estéticos (Herminio Amorim Center of Plastic Surgery and Aesthetic Treatments), Lavras, SP, Brazil.
2. Medical student at Faculdade de Medicina de Barbacena (Barbacena Medical School), Barbacena, MG, Brazil.
Correspondence to:
Hermínio da Cunha Amorim Filho
Rua Joaquim Gualberto Costa, 12 - Jardim da Glória
Lavras, SP, Brazil - CEP 37200-000
E-mail: amorim@uol.com.br
Article submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 23, 2012
Article accepted: May 5, 2012
Study carried out at Núcleo Hermínio Amorim de Cirurgia Plástica e Tratamentos Estéticos (Herminio Amorim Center of Plastic Surgery and Aesthetic Treatments), Lavras, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter