

Ideas and Innovation - Year 2012 - Volume 27 -
Extended reverse abdominoplasty
Abdominoplastia reversa estendida
ABSTRACT
Extended reverse abdominoplasty is a procedure that widens reverse abdominoplasty and was first published in 1972. The original technique is selectively used for resection of the excessive skin located in the epigastrium, and involves a single continuous cicatricial line along the inframammary crease, which crosses the sternal region. In the original technique, excess skin in the hypogastrium is resected by using lower pubic transverse abdominoplasty. This second maneuver produces 2 transverse scars, without mobilizing the bellybutton. Extended reverse abdominoplasty aims at improving the aesthetics of the entire inner wall of the abdomen through ample dissection reaching the pubis, with mobilization of the pedicle of the bellybutton. This procedure was used in a young woman who had saggy skin associated with adipose deposits and a vertical scar in the medial line of the epigastrium after bariatric surgery. Ample dissection of the abdominal cutaneous flap with mobilization and reimplantation of the bellybutton allowed aesthetic improvement of the entire anterior abdominal wall, with a single transverse scar along the inframammary crease and elimination of the scar from previous bariatric surgery. The surgery was combined with mastopexy and liposuction in the abdomen.
Keywords: Abdomen/surgery. Bariatric surgery. Weight loss. Obesity. Plastic surgery/methods.
RESUMO
A abdominoplastia reversa estendida é um procedimento que amplia a abdominoplastia reversa, publicada pela primeira vez em 1972. A técnica original é seletiva para a ressecção dos excessos cutâneos localizados no epigástrio, que determina uma única linha cicatricial contínua ao longo do sulco inframamário, cruzando a região esternal. Ainda na técnica original, os excessos cutâneos no hipogástrio são ressecados mediante abdominoplastia tipo transversal pubiana baixa. Essa segunda manobra determina duas cicatrizes transversais, sem mobilização do umbigo. A abdominoplastia reversa estendida tem o propósito de determinar melhoria estética de toda a parede anterior do abdome, mediante ampla dissecção, que atinge o púbis, com mobilização do pedículo do umbigo. O procedimento foi utilizado em uma paciente jovem, pós-cirurgia bariátrica, apresentando flacidez associada a depósitos adiposos, com uma cicatriz vertical na linha média do epigástrio. A ampla dissecção do retalho cutâneo do abdome, com mobilização e reimplante do umbigo, determinou melhoria estética de toda a parede abdominal anterior, com uma única cicatriz transversal ao longo do sulco inframamário e eliminação da cicatriz da cirurgia bariátrica prévia. O ato operatório foi combinado com mastopexia e lipoaspiração do abdome.
Palavras-chave: Abdome/cirurgia. Cirurgia bariátrica. Perda de peso. Obesidade. Cirurgia plástica/métodos.
When extended reverse abdominoplasty was first published in 19721, under the title of abdominoplasty through submammary incision, the aim of this technique was to improve the aesthetics of the abdominal segment above the horizontal line, at the level of the bellybutton, without transposing this structure. For cases in which the hypogastrium was enlarged, whether associated with saggy skin or not, the authors proposed a pubic transverse incision, similar to those performed in conventional abdominoplasties. This method produced 2 transverse scars at different levels. One lane of transversely positioned cutaneous tissue roughly 6-10 cm in size, which contained the bellybutton and its pedicle, was not dissected to preserve vascularization of the skin flaps.
In this article, we report the execution of reverse dissection of the cutaneous flap down to the pubic area for inclusion of maneuvers practiced in lower pubic transverse abdominoplasty with simultaneous umbilicoplasty.
METHOD
Clinical Aspects
We report the case of a 22-year-old nulliparous Caucasian woman who underwent a bariatric surgery 2 years ago. After a loss of 52 kg from a previous surgery, her weight was 68 kg at the time of this surgery, which had been stabilized for 4 months. The patient had no history of tobacco or alcohol use.
Physical examination showed a 19 cm-long vertical scar in the medial line of the epigastrium, which was a consequence of a previous celiotomy, as well as a few stretch marks and lipodystrophy of the flanks and entire anterior abdominal wall, predominantly in the hypogastrium.The breasts showed ptosis, with sizes in proportion to the patient's height and weight (Figure 1).
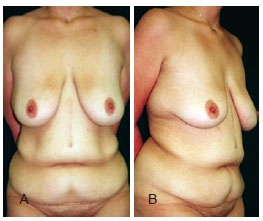
Figure 1 - A 22-year-old nulliparous patient who lost 52 kg after a previous bariatric surgery had a 19-cm scar in the middle line of the epigastrium. She weighed 68 kg at the time of the surgery; this weight had stabilized for 4 months. Mammary ptosis was present with no hypertrophy and lipodystrophy with saggy skin in the abdomen and flanks. In A, anterior view. In B, semi-lateral view.
Surgical Technique
The surgery was performed using an endotracheal tube under general anesthesia. The operative preparations involved all routine measures, including thromboembolism prophylaxis without specific medications.
The surgery started with mammoplasty, followed by liposuction complemented with abdominoplasty. Mammary pexia without reduction of volume following the Pitanguy technique2 was performed with the patient's trunk elevated (by roughly 50º), until the bilateral assembly phase, and without exteriorizing the papillary-areolar complex (Figures 2 and 3). Isolated stitches were applied using black non-absorbable monofilament 2-0 thread for fixation of the posterior side of the breasts in the chest fascia.
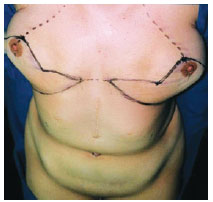
Figure 2 - Mammary markings for mastopexy using the Pitanguy technique, with the union of the inframammary incision in the sternal midline.

Figure 3 - Appearance of the bilateral assembly of the breasts, without definitive reposition of the papillary-areolar complex, as well as dissection of the abdominal skin flap, liberation of the umbilical scar and incision in the medial line until the lower limit of the scar from a previous bariatric surgery.
Next, the patient was placed in a horizontal supine position, and liposuction was performed after infiltrating all of the premarked regions of the abdomen, pubis, and flanks by using 0.9% saline solution containing epinephrine at 1: 500.000 UI, totaling 700 ml.
Liposuction was performed as follows: in the anterior wall of the abdomen, pubis, and flanks, 4-mm diameter tubes were used to suction 80% of the total aspirated volume, and the remaining 20% was complemented using 3-mm tubes in the same area. The total liposuctioned volume was 3.6 L of fat, which corresponded to 5.12% of the body weight of the patient.
Extended reverse abdominoplasty comprised a bilateral incision in the inframammary crease until the anterior axillary line, with the union in the middle sternal line. This was followed by skin dissection in the plane of the aponeurotic muscle in all of the extension of the epigastrium, bilaterally limited by 2 convergent lines until the level of the bellybutton, with the shape of an inverted triangle. Afterwards, incision of the cutaneous flap was made throughout the complete previous medial vertical scar, forming 2 half-segments extending to its caudal end (Figure 4).
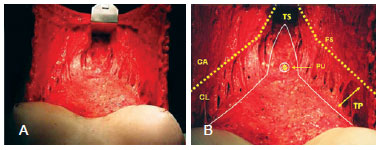
Figure 4 - In A and B, details of the abdominal skin flap are shown, which was dissected until the pubic area, with a triangular shape and the base along the inframammary line. Successive and bilateral divulsions with dilators of Dilson Luz were applied along the limits of the non-dissected skin flap. Dissection in the hypogastrium was stopped 2 cm from the external border of the rectus abdominus. The white line indicates the dissection limits. The pedicle of the bellybutton had its ends free in an island of skin of about 1 cm in diameter. FS = fascia of Scarpa. TS = selective tunneling. TP = progressive tunneling. PU = umbilical pedicle.
The bellybutton was dissected with a small ellipsoidal skin line, with a diameter of roughly 1 cm at its end. Infraumbilical dissection was performed down to the pubis, bilaterally limited about 2 cm before the lateral border of the rectus abdominus muscles (Figures 3 and 4). Subsequently, bilateral liberation throughout the entire length of the non-dissected skin flap with progressive dilation by using Dilson Luz3 valves was performed (Figure 5).
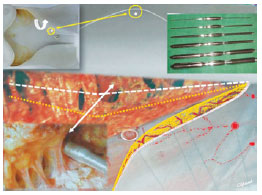
Figure 5 - Dilators of Dilson Luz with several calibers are shown, which were used for selective divulsion of the liposuctioned cutaneous cover from the lamellar to the areolar plane, with better preservation of the blood vessels, without preservation of fascia of Scarpa.
No folding of the rectus abdominus was performed. The patient was then placed with her upper body elevated (by about 20º) and the skin flaps were pulled cranially while the excess tissues were dissected, with bilateral repair stitches being applied in the sternal and inframammary regions (Figures 6 and 7). Surgical complementation was performed using umbilicoplasty and passage of adhesion stitches in the entire dissected abdominal area.

Figure 6 - Cutaneous bi-parted and cranially pulled flap, with the area of the bellybutton sutured and the excess tissues ready for dissection.
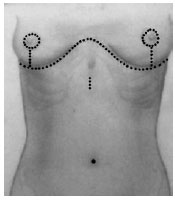
Figure 7 - Schematic representation of the suture line along the inframammary crease, crossing the sternal medial line. The previous bellybutton orifice, which was sutured, and the new positioning of the bellybutton in the skin are shown.
The papillary-areolar complexes were repositioned and sutured with isolated stitches by using non-absorbable 5-0 thread. The final suturing was performed using isolated stitches using non-absorbable 3-0 and 4-0 thread in the subcutaneous and dermal planes and absorbable 4-0 thread (polyglecapone-25) in the cuticular plane, along the sternal and inframammary lines. In the junction of the inverted T suture line, 1 stitch of a deep non-absorbable 2-0 thread was applied on both sides of the periosteum.
Drains and vacuums were inserted through the liposuction access paths. Porous adhesive tape was applied throughout the entire abdominal region and aspirated areas. In the operating room, the patient was dressed in an elastic truss for the breasts and upper body.
The drains were removed 24 h after the operation. The patient was hospitalized for the next 48 h, and the use of a corset-type girdle down to the middle upper part of the thighs was recommended for 30 days.
DISCUSSION
Ample dissection of the abdominal skin flap with mobilization and re-implantation of the bellybutton resulted in elimination of the scar from previous bariatric surgery and aesthetic improvement of the entire anterior abdominal wall, with a single transverse scar along the inframammary crease (Figures 8).
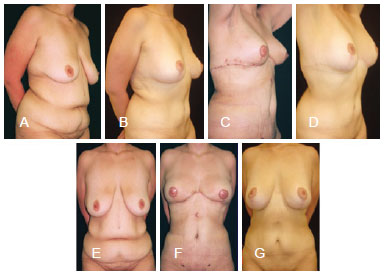
Figure 8 - In A, semi-lateral preoperative view. In B, appearance in the 18th month after the operation, which included liposuction, mastopexy, and extensive reverse abdominoplasty. In C, on the 7th postoperative day. In D, on the 18th postoperative month. In E, anterior preoperative view. In F, on the 7th postoperative day. In G, on the 18th postoperative month.
In contrast to conventional lipoabdominoplasty, in which the lipoplasty is performed in the areolar plane, in the case reported here, lipoplasty was carried out in the lameller plane and gradually reduced to the areolar plane, obtaining the desired thickness without the care needed for preservation of the fascia of Scarpa (Figure 5). The use of 4-mm tubes for 80% of the total aspirated volume and 3-mm tubes for the remaining 20% in the same areas was aimed at obtaining better uniformity in the thickness of the cutaneous flap and finalizing the procedure.
The flap was amply mobilized and pulled towards the cranial side in the present case; the vertical scar from previous bariatric surgery was eliminated and the excessive skin was resected. Treatment of the aponeurotic muscle wall was not performed because the patient had not had any pregnancies. Umbilicoplasty was carried out routinely under direct vision.
Previous studies, including skin dissections of the abdominal wall4-6, microdissections in corpses7, and non-invasive Doppler ultrasonographies8, have provided data on the qualitative and quantitative fluxometry of the circulation in the pre- and postoperative periods. Two technical details were added to the association of abdominoplasties with liposuction in a single surgery: preservation of a closed vascular system9 and selective tunneling10.
Several factors of the procedure presented in the current report are favorable:
in the lamellar layer, the perforant vessels have higher caliber because they are closer to their origin and, therefore, are at a low risk of being damaged; the adipose layer of the middle and lower segments of the abdomen is thicker and, consequently, the blood vessels are more extensive; that associated with nonpreservation of fascia of Scarpa and with the release of the non-dissected flap with dilators of Dilson Luz, offered greater mobilization of the flap (Figures 5 and 6); after liposuction of the lamellar layer, these vessels offer better circulatory guarantees, besides allowing better mobilizing conditions for the skin flap, making it more flexible, because it does not preserve the Scarpa fascia to be divulsed with the metallic valves; the ex-obese show the internal characteristics similar to those of the obese, in that the caliber and length of the vessels do not return completely to pre-obesity conditions; therefore, these patients maintain intense circulatory flow, contributing to the vitality of the cutaneous flap; limited liposuction in the areolar layer allows less manipulation in the peripheral circulatory network5, reducing the incidence of lesions in the skin vessels, besides offering less risk for the appearance of irregularities in the abdominal wall.
At the end of the dissection, a skin flap with an inferolateral pedicle was obtained, maintained by most of the vessels that comprised the three circulatory systems bilaterally, which were distributed in the lower segment of the abdominal wall and constituted of the following: (1) perforant branches of the lower epigastric arteries, as the major cutaneous source, that emerge from the sheath of the rectus muscles; (2) perforant branches constituted for anastomosis of lumbar arteries, deep iliac circumflex arteries, remnants of the intercostal arteries and remnants of the subcostal arteries that emerging from the external oblique fascia: (3) inferior superficial epigastric arteries; superficial iliac circumflex arteries; external superficial pudendal arteries; originating from the femoral arteries (Figure 9).
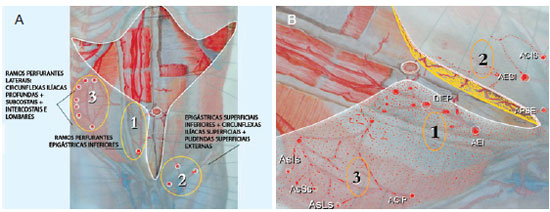
Figure 9 - In A and B, a schematic appearance of the vascular complex of the abdominal skin flap. Region 1: perforant branches of the epigastric arteries (AEI-DIEP). Region 2: lower superficial epigastric artery (AESI); superficial iliac circumflex arteries (ACIS); and external superficial pudendal artery (APSE). Region 3: deep iliac circumflex arteries (ACIP); the lumbar arteries (AsLs); remains of the subcostal arteries (AsSs); remains of the intercostal arteries (AsIs).
No signs of edema were noted, besides the ones routinely seen in conventional abdominoplasties. Adhesion points, applied within the systematization11, played 3 roles: seroma prevention, an anti-gravitational action, and a direction to the flap in the convergent ascension for the median region.
Extensive reverse abdominoplasty, whether combined with other compatible surgeries in a single operation or not, is a viable and safe procedure. Despite ample dissection, the skin flap is founded on an extensive vascular complex, making it vital and well-vascularized. The aesthetic result reflects on the entire anterior abdominal region. The procedure does not require the use of other techniques, like an anchor, or other procedures producing a second low transverse scar in the pubic area for aesthetic treatment of the hypogastrium.
This procedure is particularly compatible with reduction mammoplasty, mastopexy, and liposuction in a single operation, preferably without changing between the supine and prone positions.
REFERENCES
1. Rebello C, Franco T. Abdominoplastia por incisão submamária. Rev Bras Cir. 1972;62:249-52.
2. Pitanguy I. Mamoplastia: estudo de 245 casos consecutivos e apresentação de técnica pessoal. Rev Bras Cir. 1961;42:201-20.
3. Luz D. Técnica Dilson Luz. Tunelizações sucessivas: princípios, aplicações e procedimentos complementares. São Paulo: DiLivro; 2010.
4. Boyd BJ, Taylor GI, Corlett R. The vascular territories of the superior epigastric and deep inferior epigastric systems. Plast Reconstr Surg. 1984;73(1):1-16.
5. Taylor GI, Palmer JH. The vascular territories (angiossomes) of the body: experimental study and clinical applications. Brit J Plast Surg. 1987;40(2):113-41.
6. Munhoz AM, Ishida LH, Montag E, Sturtz G, Rodrigues L, Ferreira MC. Perfurator vessels anatomy and principal application in their inferior epigastric perfurator (DIEP) flap. Kongs Verein Deutsch Plast Chirs. 2001;32(1):1-2.
7. El-Mraky HH, Milner RH. The vascular anatomy of the lower anterior abdominal wall: a microdissection study on the deep inferior epigastric vessels and the perforator branches. Plast Reconstr Surg. 2002;109(2):539-43.
8. Fischer M, Bark A, Loureiro ALRS, Pianowski R, Graf R, Grillo MA, et al. Estudo de doppler fluxometria em retalho de abdominoplastia. ACM arq catarin med. 2003;32(Supl 1):173-8.
9. Avelar JM. Uma nova técnica de abdominoplastia: sistema vascular fechado de retalho subdérmico dobrado sobre si, combinado com lipoaspiração. Rev Bras Cir. 1999;6:3-20.
10. Saldanha OR, Pinto EB, Matos WN Jr, Lucon RL, Magalhães F, Bello EM. Lipoabdominoplasty without undermining. Aesthet Surg J. 2001;21(6):518-26.
11. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Plast Surg J. 1998;18(6):439-41.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, São Paulo, SP, Brazil.
2. Plastic surgeon, full member of the SBCP, Campinas, SP, Brazil.
3. Student of Medicine, São Paulo, SP, Brasil.
Correspondence to:
Cecin Daoud Yacoub
Av. República do Líbano, 1268 - Ibirapuera
São Paulo, SP, Brazil - CEP 04502-001
E-mail: cecinyacoub@terra.com.br
Article submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 14, 2011
Article accepted: January 24, 2012
Study carried out at the private clinic of the author, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter