ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Thoracodorsal fasciocutaneous flap in the treatment of hidradenitis suppurativa: a case report and literature review
Retalho fasciocutâneo toracodorsal no tratamento cirúrgico da hidradenite supurativa: relato de caso e revisão de literatura
Original Article -
Year2012 -
Volume27 -
Issue
1
Janete Clívea Eleutério de Oliveira Teixeira1; Afonso de Souza Ribeiro Filho2; Oscar Costa de Castro3
ABSTRACT
Hidradenitis suppurativa also known as Verneuil's disease is a chronic inflammatory and recurrent disease that occurs in the apocrine glands. It results in recurrent abscesses with purulent secretion, fistulae formation, unaesthetic and retractable scars. The most common sites involved include the axilla, inguinoperineal regions, nipple-areolar complex, and umbilicus. Here, we report a case of severe Verneuil's disease of the axillary region managed with wide excision surgery, and thoracodorsal fasciocutaneous flap and bilateral coverage. This method provides good results for reconstruction of the axillary region.
Keywords:
Apocrine glands. Hidradenitis. Axilla.
RESUMO
A hidradenite supurativa, também conhecida como doença de Verneuil, é uma inflamação crônica e recorrente das glândulas apócrinas, sem etiologia conhecida, que evolui frequentemente com saída de secreção purulenta, formação de fístulas, cicatrizes inestéticas e retráteis, podendo acometer região inguinal, axilar, aréolas mamárias e umbigo. Neste trabalho, é apresentado um caso grave de doença de Verneuil em região axilar, em que foi realizada exérese da lesão e reconstrução com retalho fasciocutâneo toracodorsal bilateral como uma opção de reconstrução da região axilar, com boa resolubilidade e resultado estético.
Palavras-chave:
Glândulas apócrinas. Hidradenite. Axila.
INTRODUCTION
Hidradenitis suppurativa is a chronic and recurrent inflammation of the skin and subcutaneous tissue; it originates from the apocrine glands and is characterized by suppuration and mucopurulent secretion, fistulae, unaesthetic scars, and cicatricial retractions1-3. This disease was first described in 1864 by Verneuil, a surgeon who identified the involvement of sweat glands in the pathophysiology of this disease, which affects only the axillae, inguinogluteoperineal, and submammary regions as well as the navel. His description resulted in the disease being called Verneuil's disease2,3. In 1922, Schiefferdecker classified the sweat glands as eccrine and apocrine, and identified the disease in apocrine glands, which is why it started to be called hidradenitis suppurativa4.
Although the etiology of this disease is not completely known, the involvement of some predisposing factors are known, such as diabetes, smoking, immunosuppression, and wearing tight clothes3,4.
Verneuil's disease primarily affects Caucasian women in their thirties. As the disease acts on apocrine glands, it only appears after puberty once these glands develop. In women, the disease predominantly involves the axillary, submammary, and inguinal regions, whereas in men, it commonly affects the perineal region4.
Here, we report a case of a male patient with bilateral axillary lesions induced by severe hidradenitis suppurativa who experienced several relapses and underwent treatment with extended surgical excision and local reconstruction.
CASE REPORT
A male Caucasian patient, 31 years old, had a history of recurrent infection in the axillary region with purulent secretion for about 7 years. He reported progressive lesion worsening and unaesthetic scar formation in addition to cicatricial retraction that limited the normal movements of the arms. He also reported that infections had become more frequent in the last year. The patient reported that in the past, he had already undergone several surgical draining procedures, although he observed only immediate results as various antibiotics were administered during moments of crisis. The patient did not use immunosuppressive drugs or present with any other immunosuppressive factors.
Upon physical examination, the patient presented with extensive suppurative lesions in both axillae in various stages of evolution along with erythematous nodules, unaesthetic and retractable scars, and foci of active infection with purulent secretion.
In May 2008, the patient received preoperative antibiotic treatment for 7 days with ciprofloxacin 500 mg, which led to improvement of the infection. The surgery was performed at the General Hospital of Fortaleza with bilateral extensive excision of the affected area followed by complete covering of the excised area with bilateral thoracodorsal fasciocutaneous flaps. The patient exhibited good clinical postoperative evolution.
The patient experienced a small local relapse 2 years after the surgery in the region in which there was still follicular proliferation on the left side around the flap; this was resolved with new resection and primary suturing.
There have been no new relapses thus far, and the esthetic results are considered good without any limitation to arm movement.
Description of the technique
The affected region was removed along with the fat layer extending to the fascia to extirpate the local apocrine glands. A 90° rotational fasciocutaneous flap in a 3:1 proportion was made on the basis of irrigation of the thoracodorsal artery.
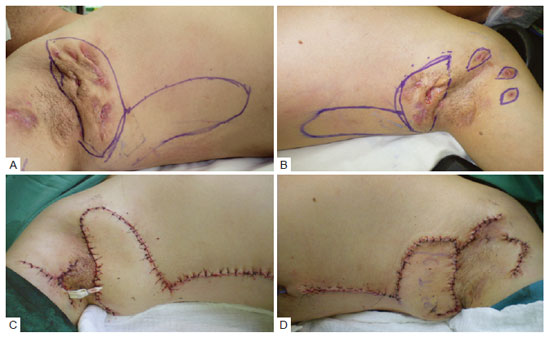
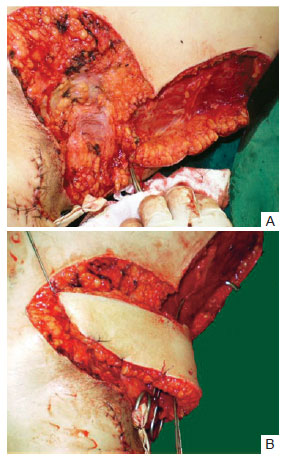
After excision of the marked area (Figure 1), the fascia were dissected (Figure 2A), turning the flap into the recipient area (Figure 2B). The primary closure of the donor area and flap suture in the axilla was subsequently executed.
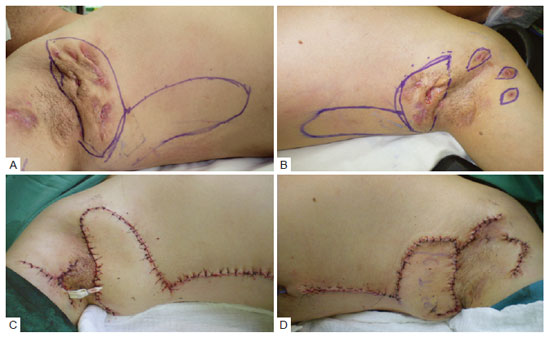
Figure 1 - In
A, preoperative lesions on the right side and flap markers. In
B, preoperative lesions on the left and flap markers. In
C, immediate postoperative image of the right side. In
D, immediate postoperative image of the left side.
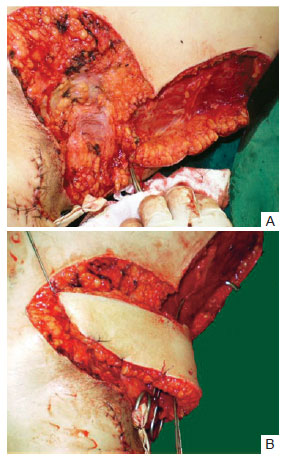
Figure 2 - In
A, dissection of the flap from the fascia. In
B, rotation of the flap in a 1:3 proportion.
DISCUSSION
The pathophysiology of Verneuil's disease involves the obstruction of the apocrine glands, resulting in glandular dilatation, bacterial infection with abscess formation and consequent rupture, tissue injury, fistula formation, fibrosis, and retractable scars5.
Conservative and surgical treatments can be used to resolve hidradenitis suppurativa. However, conservative treatment in cases of relapse has proven to be mostly ineffective, increasing relapse rates. Similarly, frequent local drainage can generate unaesthetic and cicatricial retraction with movement limitations6.
Soldin et al.7 compared 3 types of axillary resections of the lesion described above for a total of 64 operated axillae. They evaluated simple excision until the eruption of the folliculi and simple closure, and excision of the lesion and entire area with follicular proliferation until the fascia followed by grafting. Finally, they considered a wide excision with a 2-cm margin in addition to the follicular proliferation up to the fascia and followed by the flap. They found that lower rates of relapses and complications occurred when a wide resection followed by local flap was performed.
The main goal in the treatment of Verneuil's disease is complete resolution without local relapse. To ensure the achievement of this aim, the most important factor to be considered is the extensive resection of the lesion with the excision of the entire area of follicular proliferation; this is because insufficient debridement is the principal cause of high relapse rates7-10.
The three-dimensional architecture of the axillary fossa, whose shape changes with respect to movement, is a challenge for the surgeon as it must be covered using a large local flap without retractable scars6,7.
Giovannini and Giannasi8 defend the use of the parascapular fasciocutaneous flap in axillary Verneuil's disease due to the better flap quality, including lower thickness and less morbidity of the donor area. The use of skin grafts involves more relapses and retractions, resulting in movement limitations. Giovannini and Giannasi also claim that the best approach to prevent relapse is wide excision. However, they did not perceive any differences between musculocutaneous and fasciocutaneous flaps in the cases of relapse. Keeping with this notion, they prefer the fasciocutaneous flap because the transfer of musculocutaneous flaps involves a more complex technique and is restricted by the area to be covered.
Geh and Niranjan9 defend the advanced double-opposing V-Y fasciocutaneous flap as an alternative method for axillary reconstruction. Rehman et al.10 demonstrate that a single advancement in V-Y based on a consistent vascularization of the musculocutaneous thoracodorsal artery is sufficient to close the entire region of axilla follicular proliferation upon excision.
The fasciocutaneous flaps consist of skin, subcutaneous fat, and deep fascia, which are abundant during their creation in monobloc. These flaps are provided with additional blood supply that is closely associated with the underlying muscle fascia11; in the case of the flap used in this report, the supply is based on the thoracodorsal artery.
Rotational thoracodorsal fasciocutaneous flap is a practical and reliable technique that can be applied locally for regional cover. This flap presents good quality texture and has a similar color to the axillary region. Moreover, the donor area can be primarily closed. In a 1:3 proportion, this flap possesses excellent fasciocutaneous vascularization with rich anastomoses, easy dissection, less tissue thickness, and safety upon lifting.
We conclude that there are several alternatives to covering the axillary region in cases of large resections in Verneuil's disease. Most authors5-10 defend the wide resection of the entire area of follicular proliferation in order to prevent relapse.
REFERENCES
1. Paletta FX. Hidradenitis suppurativa: pathologic study and use of skin flaps. Plast Reconstr Surg. 1963;31:307-15.
2.Altmann S, Fansa H, Schneider W. Axilary hidradenitis suppurativa: a further option for surgical treatment. J Cutan Med Surg. 2004;8(1):6-10.
3. Rompel R, Petres J. Long-term results of wide surgical excision in 106 patients with hidradenitis suppurativa. Dermatol Surg. 2000;26(7):638-43.
4.Kagan RJ, Yakuboff KP, Warner P, Warden GD. Surgical treatment of hidradenitis suppurativa: a 10-years experience. Surgery. 2005;138(4):734-40.
5. Tanaka A, Hatoko M, Tada H, Kuwahara M, Mashiba K, Yurugi S. Experience with surgical treatment of hidradenitis suppurativa. Ann Plast Surg. 2001;47(6):636-42.
6.Schwabegger AH, Herczeg E, Piza H. The lateral thoracic fasciocutaneous island flap for treatment of recurrent hidradenitis axillaris suppurativa and other axillary skin defects. Brit J Plast Surg. 2000;53(8):676-8.
7. Soldin MG, Tulley K, Kaplan H, Hudson DA, Grobbelaar AO. Chronic axillary hidradenitis: the efficacy of wide excision and flap coverage. Br J Plast Surg. 2000;53(5):434-6.
8. Giovannini UM, Giannasi S. Fasciocutaneous flap to treat Verneuil disease (hidradenitis suppurativa) in the axillary region. Ann Plast Surg. 2003;50(1):108-9.
9.Geh JL, Niranjan NS. Perforator-based fasciocutaneus island flaps for the reconstruction of axillary defects following excision of hidradenitis suppurativa. Br J Plast Surg. 2002;55(2):124-8.
10. Rehman N, Kannan RY, Hassan S, Hart NB. Thoracodorsal artery perforator (TAP) type I V-Y advancement flap in axillary hidradenitis suppurativa. Br J Plast Surg. 2005;58(4):441-4.
11. Bonatto A, Arantes HL, Henriquez SS. Retalhos fasciocutâneos. In: Mélega JM, Baroudi R, eds. Cirurgia plástica: fundamentos e arte. Princípios gerais. Rio de Janeiro: Medsi; 2003. p. 142-53.
1. Aspiring training member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, resident medical doctor at the Plastic Surgery Service of the Hospital Geral de Fortaleza (General Hospital of Fortaleza), Fortaleza, CE, Brazil.
2. Full member of SBCP, preceptor of Medical Residency in Plastic Surgery at the Hospital Geral de Fortaleza (General Hospital of Fortaleza), Fortaleza, CE, Brazil.
3. Full member of SBCP, Head of Clinic and Regent of the Plastic Surgery Service at the Hospital Geral de Fortaleza (General Hospital of Fortaleza), Fortaleza, CE, Brazil.
Janete Clívea Eleutério de Oliveira Teixeira
Rua Frei Mansueto, 303 - ap. 1002
Fortaleza, CE, Brazil - CEP 60175-070
E-mail: janeteclivea@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 6, 2010
Article accepted: October 18, 2010
Study conducted at the Plastic Surgery Service of the Hospital Geral de Fortaleza (General Hospital of Fortaleza), Fortaleza, CE, Brazil.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license