ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Augmentation gluteoplasty: experience at Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service
Gluteoplastia de aumento: experiência do Serviço de Cirurgia Plástica Dr. Ewaldo Bolivar de Souza Pinto
Original Article -
Year2012 -
Volume27 -
Issue
1
Daniel Melo de Azevedo1; Paulo Gonçalves Junior2; Juliano Pereira2; Tiago Boulhosa Amoedo2; Fábio Massaru Kuroyanagi2; Emm anuel Francis Mallol Cotes3; Ewaldo Bolivar de Souza Pinto4; Osvaldo Ribeiro Saldanha5
ABSTRACT
BACKGROUND: The buttocks are formed by muscles responsible for leg movement, the largest being the gluteus maximus. Moreover, the buttocks have secondary sexual function: they are an erogenous area and a symbol of fertility, and are employed in advertising for male-oriented consumer products. Women with bigger buttocks arouse greater attraction and sexual desire, which has driven the demand for augmentation gluteoplasty with silicone implants. This study analyzed the authors' experience with the XYZ augmentation gluteoplasty technique by comparing the rates of complications related to the procedure between gluteoplasty + back and flank liposuction, and gluteoplasty alone.
METHODS: A total of 8 women were subjected to XYZ augmentation gluteoplasty between July and November 2011. The patients were divided into 2 groups with 4 members each. In groups 1 and 2, gluteoplasty with and without liposuction of the back and flanks was performed, respectively.
RESULTS: Four, 2, and 2 pairs of 400-, 350-, and 300-mL Quartzo® implants were used, respectively. The total incidence of seroma, necrosis of the edges, and wound dehiscence was 50% (4 cases in total) in both groups.
CONCLUSIONS: XYZ augmentation gluteoplasty with silicone implants produces natural and long-lasting results with low complication rates when not combined with liposuction.
Keywords:
Buttocks/surgery. Prosthesis implantation. Prostheses and implants.
RESUMO
INTRODUÇÃO: As nádegas são constituídas por músculos responsáveis pelos movimentos das pernas, assumindo o músculo glúteo máximo o volume principal. Possuem uma função secundária, de cunho sexual, como zona erógena, símbolo de fertilidade, cujo poder de atração é um forte apelo usado pela publicidade de artigos de consumo masculino. Mulheres com maior volume de nádegas despertam maior atração e desejo sexual, o que tem levado ao aumento da procura pela gluteoplastia de aumento com utilização de implantes de silicone. O objetivo deste trabalho é demonstrar a experiência dos autores com a técnica de gluteoplastia de aumento XYZ, comparando as taxas de complicação relacionadas ao procedimento entre dois grupos, gluteoplastia + lipoescultura de dorso e flancos vs. gluteoplastia isolada.
MÉTODO: No total, 8 pacientes do sexo feminino foram submetidas a gluteoplastia de aumento pela técnica XYZ, no período entre julho e novembro de 2011.
RESULTADOS: Foram utilizados 4 pares de implantes com volumes de 400 ml, 2 pares de 350 ml e 2 pares de 300 ml, todos do tipo Quartzo®. As pacientes foram divididas em dois grupos, com 4 integrantes cada. No grupo 1, a gluteoplastia foi associada a lipoaspiração de dorso e flancos; no grupo 2, não foi feita essa associação. A incidência total de seroma, necrose das bordas e deiscências das feridas foi de 50% (4 casos) cada.
CONCLUSÕES: A gluteoplastia de aumento pela técnica XYZ com utilização de implantes de silicone tem produzido resultados naturais e de longa duração, com baixas taxas de complicação quando não se associa lipoaspiração.
Palavras-chave:
Nádegas/cirurgia. Implante de prótese. Próteses e implantes.
INTRODUCTION
The contour of the body is enormously important in the daily practice of a plastic surgeon. Liposuction plays a critical role in approaches involving the posterior part of the body. Liposuction with or without fat grafting has several limitations related to the proper modeling of the buttocks, which is the most important region affecting the posterior body contour. The buttocks are the 2 prominent globular areas located on the back of the pelvis, bounded by an imaginary line that passes above the highest point of the iliac crests until the intergluteal groove. The gluteus maximus muscle is the largest of its muscles; however, in the anterolateral region, the superficial gluteus medius contributes to the contour of this body part. Moreover, the buttocks have secondary sexual functions as an erogenous area and an ancient symbol of fertility. Nowadays, their attractiveness is used in advertising for male-oriented consumer products. Women with bigger buttocks arouse greater attraction and sexual desire, which has driven the increased demand for augmentation gluteoplasty with silicone implants.
Augmentation gluteoplasty may be performed using autologous tissues, i.e., tissues from the body itself (e.g., fat, skin-fat flaps, and muscular flaps) or artificial materials (e.g., implants and fillers); furthermore, these can be combined or introduced separately.
Gluteal remodeling is indicated in various situations including the repair of acquired deformities (e.g., sequelae of accidents, loss of substance, cicatricial sequelae, etc.) and congenital deformities (e.g., agenesis and incomplete development). Augmentation gluteoplasty for aesthetic purposes is performed to restore the contour, shape, and volume of the buttocks.
Gluteal implants provide an effective means for remodeling and augmenting the buttocks, which are not always obtained with other procedures. The insertion of implants by concentrated projection creates the desired round shape, which cannot always be achieved using fat grafting.
Gluteal implants can be round or oval and filled with highly cohesive or soft silicone blocks. There are 4 routes for placing gluteal implants: subcutaneous, subfascial, intramuscular, and submuscular.
In 1969, Bartels et al.1 first described augmentation gluteoplasty with subcutaneous implants. This procedure resulted in large numbers of dislocations, asymmetries, and capsular contractures.
Then, Robles et al.2 reported a new technique for gluteal augmentation by placing submuscular implants through an incision in the midline of the sacral region.
Vergara and Marcos3 published a procedure for gluteal augmentation involving an intramuscular implant, whereas De La Peña et al.4 described the placement of subfascial prostheses.
At present, there is some controversy whether the intramuscular or the subfascial plan is ideal for the positioning of gluteal implants. In countries where augmentation gluteoplasty has become popular, such as Brazil, the most popular incision plan is the intramuscular one.
Gonzalez5 describes the XYZ technique, which establishes parameters for proper intramuscular incision by marking anatomical references to guide the dissection and prevent the implants from being visible and palpable.
The aim of the present study is to detail the authors' experience with XYZ augmentation gluteoplasty.
METHODS
A total of 8 women were admitted to the plastic surgery outpatient clinic of the University of Santa Cecília (UNISANTA) and subjected to XYZ augmentation gluteoplasty between July and November 2011. All procedures were performed by third-year residents.
The women were aged between 28 and 50 years and presented with gluteal hypotrophy. Patients were divided into 2 groups with 4 members each. In group 1, back and flank liposuction was combined with gluteoplasty, while in group 2, only gluteoplasty was performed. Patients in both groups were submitted to weekly evaluation for 1 to 3 months.
The implants used for the gluteal region were Quartzo® type high-projection oval models with volumes ranging from 300 to 400 mL. Aesthetic correction of gluteal hypotrophy was the predominant indication for the surgery.
Surgical procedure
With the patient in orthostatic position, line A, which corresponded to the highest point of the intergluteal groove referring to a standing patient, was marked.
The whole surgery was based on 3 reference points: the iliac crest, and posterior-superior and trochanter iliac spines.
With the patient in ventral decubitus position, a double line 7-cm long and 4-mm wide was made from line A towards the caudal direction on the intergluteal groove. This was done to help preserve the sacro-cutaneous ligament, which is responsible for the formation of the intergluteal groove. Then, an inverted heart centered on the previously made fusiform incision was drawn. The lateral edge of the inverted heart was 7 cm from the intergluteal groove. The posterior-superior iliac spine and iliac crest were identified and separated. Then, line G, which corresponded to the lateral limit of the gluteus maximus muscle, whose cephalic part was 4 cm from the posterior-superior iliac spine, was drawn on the iliac crest. The caudal region was indicated by the face of posterior-lateral trochanter.
All patients received general anesthesia with cefalotine in the anesthetic induction. The patients were positioned in ventral decubitus position. Cushions were placed under the anterior regions of the pelvis and chest. The anus was completely isolated with a compress soaked with topical povidone-iodine solution sutured to the skin of the patient.
The whole area of the inverted heart was infiltrated with a vasoconstricting solution. The skin was incised while preserving the sacral cutaneous ligament. The subcutaneous tissue was dissected at 45º to the muscular fascia, progressing on the muscular fascia throughout the drawing area. A 6-cm incision was made in the muscle and fascia following the direction of muscular fibers from the edge of the sacrum to the bottom of the separated area. Through this incision, a fissure was created with the index finger. Point X was defined within this cleft by caudal palpation of the sacrotuberous ligament, which corresponds to half of the muscle thickness at a depth of 2.5 to 3 cm. A separator was introduced at point X in the direction of the posterior-superior iliac spine. To reach this anatomical structure, an inferior slight rotation in the direction of point Y was made. Using the muscle fibers next to the sacrum as support, a rotational movement with the tip of the separator from point Y to the more caudal point of the G line (i.e., point Z) and tangential to the posterior-lateral face of the trochanter was performed. The separation was achieved by digital maneuvering and a muscular dilator. Next, drains and implants were placed, followed by closure of the area with 2-0 nylon thread. In the region of the inverted heart, adhesion sutures and sutures at the base of the sacral-cutaneous ligament were made with 3-0 nylon thread. The skin area corresponding to the sacral-cutaneous ligament was de-epidermized. Subdermic suturing was carried out with 4-0 nylon thread. Superficially, a separated epidermal suture or simple running suture was made using 6-0 nylon thread, whereas intradermic suturing was performed with 3-0 nylon thread.
RESULTS
No intraoperative complications were observed.
The patients were placed in a high dorsal decubitus position using special cushions positioned on the back and legs to avoid compression of the separated muscle between the implant and mattress.
As postoperative analgesia, intravenous tramadol (100 mg) and codeine + oral paracetamol (30 mg/750 mg) were administered every 8 hours.
The average times of hospital admission and drainage were 24 and 48 hours, respectively.
The patients were discharged with a prescription of codeine + paracetamol (30 mg/750 mg) for 7 days.
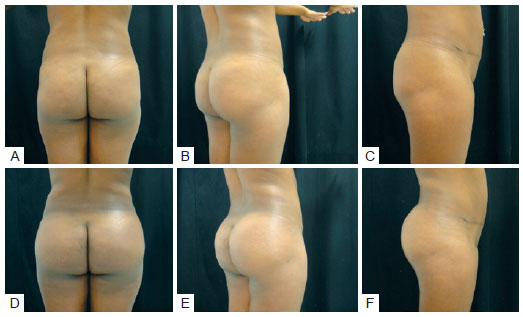
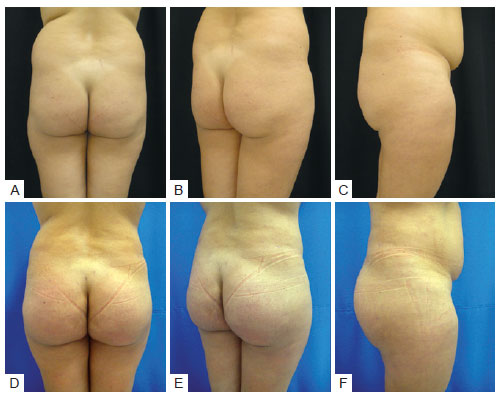
The gluteal volume of the patients increased significantly (Figures 1 to 3) with immediate and long-term satisfaction in 100% of the cases.
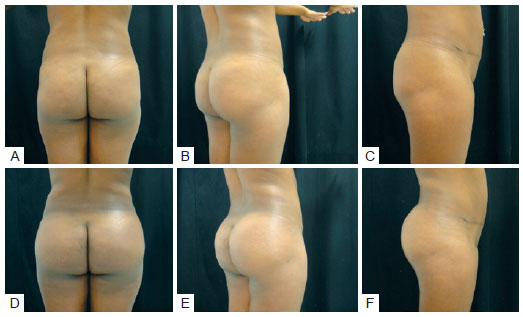
Figure 1 - Case 1. In
A, B, and
C, preoperative aspects. In
D, E, and
F, 45 days after augmentation gluteoplasty with 400-mL Quartzo
® type implants.
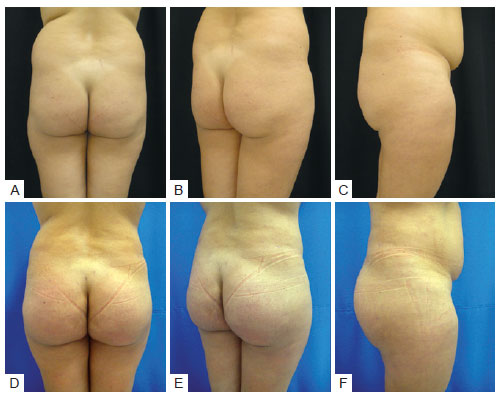
Figure 2 - Case 2. In
A, B, and
C, preoperative aspects. In
D, E, and
F, 90 days after augmentation gluteoplasty with 350-mL Quartzo
® type implants + liposuction of the back.

Figure 3 - Case 3. In
A, B, and
C, preoperative aspects. In
D, E, and
F, 60 days after augmentation gluteoplasty with 350-mL Quartzo
® type implants + liposuction of the back.
Four, 2, and 2 pairs of 400-, 350-, and 300-mL Quartzo® implants were used, respectively.
The most frequent immediate complications were pain, seroma, wound dehiscence, and infection.
Only 1 patient in group 1 requested prolonged analgesia for another week due to moderate pain.
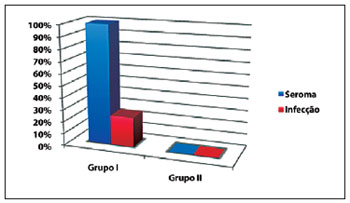
The four patients in group 1 presented with seroma with persistent drainage associated with necrosis of the edges and dehiscence of the operated wounds from 8 to 14 days after the surgery (Figures 4 and 5). These patients underwent debridement of the necrotic edges, cleaning of the wounds with povidone-iodine topical solution and 0.9% saline solution under pressure using 20-mL syringes and 40 × 12 (18-G) needles, and re-suturing. These patients showed positive evolution with resolution of the complications on day 30 after the surgery.

Figure 4 - Dehiscence of the operated wound, necrosis, and drainage of seroma 10 days after augmentation gluteoplasty combined with liposuction.
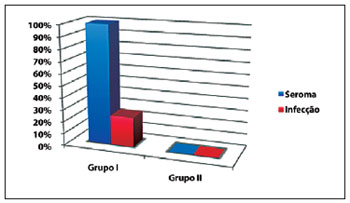
Figure 5 - Incidence of complications in augmentation gluteoplasty with intramuscular implants. Group I, gluteal implants combined with liposuction of the back. Group II, gluteal implants without liposuction of the back.
One patient in group 1 showed purulent drainage from the operated wounds and peaks of fever. Therefore, the sutures were removed from the skin, the wounds were washed with povidone-iodine topical solution and 0.9% saline solution under pressure using 20-mL syringes and 40 × 12 (18 G) needles, and re-suturing was performed. In addition, antibiotic therapy was administered using intravenous ceftriaxone and oral metronidazole for 7 days. Secretions were collected and sent for microbiological culture; no bacterial growth was observed. In 48 hours, the patient had no more fever peaks; after 15 days, the seroma was resolved.
The patients in group 2 did not present any complications.
The total incidence of seroma, necrosis of the edges, and dehiscence of the wounds was 50% (4 cases) in both groups.
No cases of muscular atrophy, visible or palpable implants, or dislocations were observed.
DISCUSSION
The placement of gluteal implants using the subcutaneous and subfascial plans may result in the implants being visible. In the submuscular plan, due to the proximity of the sciatic nerve, the caudal separation should not extend beyond the bottom edge of the pyramidal muscle. This restricts the location of the implant above the buttocks, giving the impression of a "double-buttock" especially in patients with long buttocks. With the intramuscular plan, the coverage provided in this region is sufficient to hide the implant.
Vergara and Marcos3 described the intramuscular plan, aiming to place the implant in a lower position, although anatomical references for the intramuscular separation were not safely established.
The intramuscular plan has 2 disadvantages: the difficulty of muscle separation in the correct plan, which can lead to a visible and palpable prosthesis, and intense pain in the immediate postoperative period.
Gonzalez5 described the XYZ procedure, which provides a guide for the surgeon to determine the optimal plan for muscle dissection through the identification of anatomical references, facilitating predictable results with low complication rates.
The most frequent immediate complications are pain, wound dehiscence, seroma, and infection. Seroma may result either from dissection of the intramuscular region from the suprafascial separation performed to expose the muscle in the area of the inverted heart or from liposuction in the neighboring zones. Seromas and everted edges that trigger necrosis are the main causes of wound dehiscence.
Vergara and Amezcua6 report complications in 16 (10%) of 160 cases: seroma in 7 cases (4%), asymmetry in 4 (2.66%), capsular contracture in 3 (2%), hypercorrection in 1 (0.66%), and implant rupture in 1 (0.66%).
After 73 gluteoplasties, Mendieta7 identified wound dehiscence with persistent drainage of seroma from 8 to 14 days after surgery as the most common complication, affecting 30% of the cases. One case of infection with no need for implant removal was observed as well.
In 500 consecutive cases, Gonzalez8 reports incidences of dehiscence and infection of <10% and 1.1%, respectively.
The preservation of the sacral cutaneous ligament for the closure of the incision proposed by Gonzalez5 prevents deletion of the intergluteal groove; it also improves scarring by reducing both the incidence and severity of dehiscence. In addition, it serves as base to anchor the 2 sides of the dehiscence wound when re-suturing is required.
In the postoperative period, the dorsal decubitus position with special cushions avoids compression of the separated muscle between the implant and mattress; this minimizes neuralgia of the sciatic nerve caused by irritation triggered by serosal collection and blood cells derived from the separation of the regions.
However, in the literature, the complication rates between single and combined procedures are not differentiated.
CONCLUSIONS
Augmentation gluteoplasty with silicone prostheses using the intramuscular plan provides efficient muscular coverage of the implant as well as protection against infection. This technique maintains the position and prevents the downward migration of the implant. Moreover, it confers natural-looking and consistent results; not only does it increase the size of the buttocks, it also remodels, rounds, and firms them, achieving smooth, harmonious, and aesthetically pleasing contours without irregularities.
By marking anatomical references to guide the intramuscular dissection in the correct plan, the XYZ procedure is reproducible and avoids complications such as visible and palpable implants.
Despite the small number of cases analyzed, the 100% incidence of seroma, edge necrosis, and partial wound dehiscence when back and flank liposuction was combined with augmentation gluteoplasty discourages its use.
The high complication rates compared to those in the literature might be due to the small cohort of patients (Figure 6). Moreover, most of the work in the literature does not differentiate between single and combined procedures.

Figure 6 - Incidence of complications in augmentation gluteoplasty with intramuscular implants. SCPEBSP, Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service.
Further studies using larger and controlled numbers of patients are required in order to compare augmentation gluteoplasty with and without liposuction.
XYZ augmentation gluteoplasty with silicone implants without liposuction provides satisfactory, natural, and long-lasting results with low complication rates.
REFERENCES
1. Bartels RJ, O'Malley JE, Douglas WM, Wilson RG. An unusual use of the Cronin breast prosthesis. Case Report. Plast Reconstr Surg. 1969;44(5):500.
2. Robles JM, Tagliapietra JL, Grandi MA. Gluteoplastia de aumento: implante submuscular. Cir Plast Iberolatinoam. 1984;X:4-9.
3. Vergara R, Marcos M. Intramuscular gluteal implants. Aesthetic Plast Surg. 1996;20(3):259-62.
4. De La Peña JA, Rubio OV, Cano JP, Cedillo MC, Garces MT. Subfascial gluteal augmentation. Clin Plast Surg. 2006;33(3):405-22.
5. Gonzalez R. Augmentation gluteoplasty: the XYZ method. Aesthetic Plast Surg. 2004;28(6):417-25.
6. Vergara R, Amezcua H. Intramuscular gluteal implants: 15 years experience. Aesthet Surg J. 2003;23(2):86-91.
7. Mendieta CG. Gluteoplasty. Aesthet Surg J. 2003;23(6):441-55.
8. Gonzalez R. Gluteal implants: the "XYZ" intramuscular method. Aesthet Surg J. 2010;30(2):256-64.
1. Associated member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, intern at Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service, University of Santa Cecília (UNISANTA), Santos, SP, Brazil.
2. General Surgeon, External Intern at Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service, UNISANTA, Santos, SP, Brazil.
3. Full member of SBCP, Director of the Post-graduation Course at Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service, UNISANTA, Santos, SP, Brazil.
4. Full member of SBCP, Director of SBCP Scientific Event Department, Coordinator of Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service, UNISANTA, Santos, SP, Brazil.
Daniel Melo de Azevedo
Av. Washington Luiz, 142 - Encruzilhada
Santos, SP, Brazil - CEP 11050-200
E-mail: danihelmeloazevedo@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 28, 2011
Article accepted: March 19, 2011
Study conducted at Dr. Ewaldo Bolivar de Souza Pinto Plastic Surgery Service, University of Santa Cecília (UNISANTA), Santos, SP, Brazil.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license