

Original Article - Year 2012 - Volume 27 - Issue 1
Bipedicled TRAM flap with rectus abdominis muscle preservation below the arcuate line without reinforcing mesh
TRAM bipediculado com preservação dos músculos retos do abdome abaixo da linha arqueada e sem o uso de tela de reforço
ABSTRACT
BACKGROUND: The use of a bipedicled transverse rectus abdominis myocutaneous (TRAM) flap in breast reconstructions has required the prophylactic use of mesh in the lower segment of the hypogastrium, because of the frequency of bulging and herniations in the middle to long term. This study aims to record a technical procedure routinely used in breast reconstructions: bipedicled TRAM flap without previous autonomization, with total preservation of the rectus abdominis and pyramidal muscles in their sheaths at the limit of the arcuate line without the use of mesh, and without secondary herniation of the abdominal wall in the long term.
METHODS: Bipedicled TRAM flap, without the use of mesh and, through the preservation of both the rectus abdominis muscles in their sheaths from the arcuate line to the pubis, without the presence of bulging or herniation in the lower segment of the hypogastrium, was performed on 11 patients. The plication of the musculoaponeurotic layer in the hypogastrium followed a specific surgical routine after the migration of the rectus abdominis, with complementary suture of its aponeurosis in the respective arcuate lines, and with the necessary reinforcement to avoid either the use of mesh or the onset of bulging and herniation.
RESULTS: The aesthetic result obtained in all cases was considered satisfactory both by patients and by the surgical staff. The patients did not develop any type of secondary herniation or bulging in the abdominal wall in the postoperative follow-up period.
CONCLUSIONS: The bipedicled TRAM flap technique with preservation of the rectus abdominis muscles below the arcuate line and without the use of reinforcement mesh provides satisfactory results that are maintained in the middle to long term, without the development of any secondary herniation in the abdominal wall.
Keywords: Reconstructive surgical procedures. Mammaplasty. Breast/surgery. Surgical flaps. Abdominal muscles/surgery.
RESUMO
INTRODUÇÃO: O emprego de transverse rectus abdominis musculocutaneous (TRAM) bipediculado nas reconstruções mamárias tem requerido o uso profilático de telas no segmento inferior do hipogástrio, pela frequência de abaulamentos e hérnias, a médio e longo prazos. O presente estudo tem o objetivo de registrar um procedimento técnico utilizado de rotina nas reconstruções mamárias com TRAM bipediculado, sem autonomização prévia, com a preservação total dos músculos retos e piramidais em suas bainhas no limite da linha arqueada, sem o uso de telas e sem herniação secundária da parede abdominal a longo prazo.
MÉTODO: Utilização, em 11 pacientes, de TRAM bipediculado, sem o uso de telas e sem a presença de abaulamentos e hérnias no segmento inferior do hipogástrio, por meio da preservação de ambos os músculos retos abdominais, em suas bainhas desde a linha arqueada até o púbis. A plicatura da parede musculoaponeurótica no hipogástrio seguiu a rotina cirúrgica específica após a migração dos músculos retos abdominais, com complementação da sutura de suas aponeuroses nas respectivas linhas arqueadas, mantendo o reforço necessário para evitar o uso de tela e o aparecimento de abaulamento e hérnia.
RESULTADOS: O resultado estético obtido em todos os casos foi considerado satisfatório pelas pacientes e pela equipe cirúrgica. No acompanhamento pós-operatório, as pacientes não desenvolveram nenhum tipo de herniação ou abaulamento secundários da parede abdominal.
CONCLUSÕES: A técnica de TRAM bipediculado com preservação dos músculos retos do abdome abaixo da linha arqueada e sem o uso de tela de reforço proporciona a obtenção de resultados satisfatórios, mantidos a médio e longo prazos, sem desenvolvimento de nenhum tipo de herniação secundária da parede abdominal.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos. Mamoplastia. Mama/cirurgia. Retalhos cirúrgicos. Músculos abdominais/cirurgia.
Since the pioneering studies, both published in 1982, of Gandolfo1 and Hartrampf et al.2 on breast reconstruction with the transverse rectus abdominis musculocutaneous (TRAM) flap, the literature has continually recorded contributions by other authors, whose studies have added details that enable improvements in the safety, handling, and aesthetic quality of the results in both the donor and recipient areas. An improved knowledge of anatomy, circulation, and, particularly, the rectus abdominis muscles, has reduced the incidence of complications inherent to this type of breast reconstruction.
Despite the refinements that have been introduced and the selectivity criteria that made possible the use of microsurgery, a variety of problems still occur as a result of the actions of surgeons, patients, or both.
Diversifications in the use of mono- and bipedicled TRAM3-8 flap for unilateral and bilateral breast reconstruction, with and without previous autonomization9 of the TRAM flap, and even with microsurgery10,11 are some of the current options in use. The existence of several techniques shows that none of them is ideal for all cases of reconstruction.
One of the problems referred to in the literature is the presence of herniations and bulging in the hypogastrium, in the middle to long term, in cases where both the rectus muscles are used to prepare the TRAM flap.12,13 The incidence of this problem as reported in the literature varies; however, most authors report the complementary need for the use of mesh over the donor region, in order to limit these secondary effects. Yet the specific statistics on the use of mesh as an effective and prophylactic element have differed, because of differences in case selection and authors' experience.
This study aims to record a technical procedure routinely used in breast reconstructions: bipedicled TRAM flap without previous autonomization, with total preservation of the rectus and pyramid muscles in their sheaths at the limit of the arcuate line without the use of mesh, and without secondary herniation of the abdominal wall in the long term.
Surgical anatomy
Studies on the anatomy of the abdominal wall in the mobilization regions of the rectus abdominis muscles with regard to the morphological aspects, vascular and lymphatic circulation, innervation, and recipient bed of the new breast have been widely published. Some anatomical aspects should be highlighted:
1.The anterior and lateral walls of the abdomen are formed by a distributed muscular complex in planes, whereby the external and internal oblique, transversus abdominis, and rectus muscles, covered by their respective aponeuroses, form a containing wall for the intraabdominal organs. In the anterior midline, external oblique muscle aponeurosis, and anterior and posterior laminae of the internal oblique muscle, together with the transversus muscle, are joined to form the linea alba from the xiphoid process to the pubis. The association of the aponeurosis of the 3 lateral muscles of the abdomen extends from the ribs to the pubis along the lateral margin of each rectus muscle, forming the semilunar line. The semilunar line and the linea alba form important vertical structures of support, whose preservation should be maintained in the dissection of the rectus abdominis muscles when preparing the TRAM flap. From the arcuate line (typically positioned halfway between the umbilicus and the pubis) to the pubic crest, the posterior face of the rectus abdominis muscles are coated exclusively by their aponeurosis, transverse muscle aponeurosis, and peritoneum. This detail makes the region thinner and less resistant. During the single-pedicled TRAM flap preparation, several authors report the transverse resection of the rectus abdominis muscle with its respective sheath in order to integrate it with to the cutaneous flap, without specifying how many centimeters below the arcuate line this is done. However, all agree that for cases where both the rectus abdominis muscles are mobilized, weakening of the abdominal wall is a reality, as it is maintained only by the transverse fascia and the posterior face of the rectus abdominis muscle. Therefore, the reinforcement mesh is required to decrease the possibility of herniations in the middle to long term.
2.The understanding of rectus abdominis muscle vascularization increased after it was studied in detail after the development of TRAM flap14-16 for new breast reconstructions. The rectus abdominis muscle is supplied by the superior epigastric, inferior epigastric, and intercostal arteries. The superior epigastric artery originates from the internal thoracic artery, penetrates the abdomen about 3 cm lateral from the midline and below the costal rim, and immediately crosses the posterior sheath of the rectus abdominis muscle. It continues caudally along the middle third of the posterior face of the rectus abdominis to approximately 2 to 4 cm above the umbilical line, giving off several branches that anastomose with the branches of the inferior epigastric artery. The inferior epigastric artery originates from the external iliac artery and rises obliquely and laterally out of the rectus abdominis muscle sheath to approximately 6 cm below the arcuate line, where it emits numerous muscular branches. These branches run upward to reach the branches of the superior epigastric artery, which together form a rich vascular network that anastomoses with the one on the opposite side. Moon and Taylor,17 through a detailed vascular study, proved that the inferior epigastric artery of a vascular pedicle is dominant, constituting a greater caliber vessel to nourish the rectus abdominis muscle. However, the TRAM flap survives with the pedicle from the superior epigastric artery. Surgical attempts at previous autonomization of the TRAM to reverse the flap's blood flow are being selectively applied by several authors already mentioned. The inferior epigastric artery is used for cases of free flaps in microsurgery. Several intercostal arteries that penetrate through the lateral edge of the rectus abdominis muscle follow the nerves in a segmental manner. In TRAM flap dissection, these vessels and nerves are surgically sectioned. These studies enabled the division of the cutaneous flap according to the muscular single pedicle position into 4 zones18: zone I, the myocutaneous segment directly perfused by the perforating arteries; zone II, the segment perfused by the axial vessels that cross the midline and reach the contralateral dermal plexus; zone III, the ipsilateral segment with the muscle, perfused by the axial vessels; zone IV, the extremity of the contralateral segment, perfused from the previous dermal plexus after autonomization of the flap. Surgical practice has shown that zones I and II, and only the limit of the zone III with the zone I survive without major risk of necrosis. In order to solve this problem and have a greater utilization and vascular safety in zone IV, the TRAM flap is autonomized by surgeons who use a single muscular pedicle. Under local anesthesia and by using a small access route close to the pubis, the inferior epigastric artery is sectioned and the incision is then sutured. With this technique, the definitive surgery can usually be performed in 1 to 3 weeks.
METHODS
During the period from 2006 to 2009, 11 patients were operated on using this technique: 7 underwent immediate breast reconstruction after mastectomy and 4 were reconstructed with late TRAM flap.
Surgical technique
Markings for delimitation of the TRAM flap were made with the patient in a standing position, prior to anesthetic premedication.
The cutaneous area was in the form of a wide ellipse covering the hypogastrium, extending, in general, from one anterior superior iliac spine to the other and bounded inferiorly by the pubis, about 7 to 8 cm from the vulvar anterior commissure, and superiorly to about 1 to 4 cm above the umbilicus. These delimitations were basically similar to those used in abdominoplasties with low transverse pubic incision.
The upper limit to the umbilicus varied in distance in relation to the pubis and the cutaneous excess of the hypogastrium.
The operations were performed under general anesthesia with endotracheal intubation and the patient in the supine position. The next steps were as follows:
The skin incision was made using the marked limits and was taken through all layers up to the aponeurotic plane. In the upper extension of the incision, the incision was beveled to contain as much of the supraumbilical vascular plexus as possible. The dissection of the supraumbilical cutaneous flap was performed up to the xiphoid process and the costal arches and, laterally, up to the oblique muscles. The dissection was prolonged in the direction of the recipient bed of the new breast to form a tunnel whose dimensions were sufficient to pass the surgeon's open hand. A selective thinning of the adipose tissue along the tunnel was done, when there was excess. The next step was to mark the delimitation over the TRAM flap to estimate the projection of the rectus muscles still in the interior of their sheaths, particularly on the internal edges in order to assess them for diastasis (Figure 1).
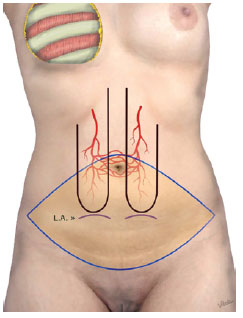
Figure 1 - Schematic appearance of the cutaneous flap delimitation in the shape of an ellipse in the hypogastric region. The scheme also illustrates the projection of both the rectus abdominis muscles, the limits of the arcuate line (usually halfway between the umbilicus and the pubis), and the periumbilical vascular plexus, between both the superior epigastric arteries.
A periumbilical skin incision, about 1 cm in diameter, and the dissection of its pedicle completely released the umbilicus from the cutaneous flap. The dissection started at the lower edge of the flap close to the pubis, throughout the aponeurotic plane up to the limit of the arcuate line, generally at half the distance between the umbilicus and the low transversal pubic incision, preserving the integrity of the rectus muscles and the linea alba. The dissection was continued bilaterally in the medial direction, following the same aponeurotic plane until the visualization of larger caliber perforating vessels, usually 1 to 2 cm medial to the semilunar line. Next, on both sides, the aponeurosis was incised transversely at 1 cm above the limit of the arcuate line, continuing laterally and medially in the cranial direction, parallel to the body of the rectus abdominis muscle to the upper edge of the incised cutaneous flap. Above the upper limit of the myocutaneous flap, the anterior aponeurosis of both the rectus muscles was incised in the longitudinal direction until the xiphoid process was approached; next, whole muscles were removed from their bed. A long Kocher clamp was passed close to the arcuate line and exteriorized on the opposite side. Next, the muscle was transversally sectioned. In the lower face of the cutaneous flap, isolated sutures with nonabsorbable thread were applied in the musculoaponeurotic layer with the flap's adipose tissue for better fixation. Both muscular pedicles with their respective aponeuroses integrated with the cutaneous flap were able to be mobilized to the recipient area (Figure 2).
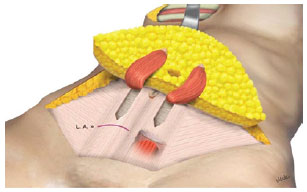
Figure 2 - Schematic appearance of the dissected and everted cutaneous flap, as well as of both the rectus muscles dissected from their beds to the limit of the arcuate line and sutured in the subcutaneous cellular tissue of the flap.
The rectus muscles' aponeuroses and their plication along the linea alba were sutured with isolated sutures of 0-Prolene, similar to the plication performed in abdominoplasties. The rectus muscle stumps and the respective aponeuroses were sutured in the arcuate line. Isolated quilting sutures19 were applied along the whole extent of the dissected cutaneous abdominal wall, from the xiphoid process to the pubis, with 2-0 or 3-0 absorbable thread. Two drains with continuous aspiration were positioned from the epigastrium and exteriorized close to the pubis. The final suture, in the entire extent of the low abdominal incision, was held with isolated threads of 2-0 Monocryl, approximating the aponeurosis and the adipose tissue. Isolated sutures were passed in the dermis and intracuticular continuous suture was performed with 3-0 Monocryl. A noncompressive dressing was applied with micropore adhesive tape directly on the suture line and cotton wad covering the operated areas.
Figure 3 illustrates the surgical details described, synthesizing the transoperative sequence of late breast reconstruction with bipedicled TRAM flap.
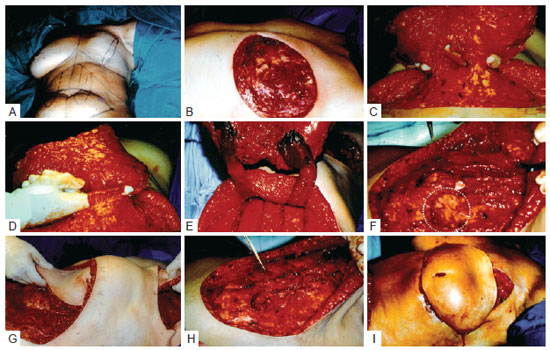
Figure 3 - Transoperative sequence of late breast reconstruction with bipedicled TRAM flap, in a 46-year-old patient who underwent mastectomy without preservation of the pectoralis major muscle. In A, Marking the cutaneous flap in the hypogastrium. In B, Exposure of the left pectoral area to receive the abdominal flap. In C, Cutaneous flap dissected with the rectus muscles still in the interior of their sheaths. In D and E, The dissected rectus abdominis muscles are ready to be sectioned, and bilaterally sutured into the subcutaneous cellular tissue of the mobilized abdominal flap. In F, The appearance of the beds and of the respective arcuate lines after mobilization of the rectus muscles, before the routine suture of the preperitoneal layers to the posterior face of the rectus muscles upstream. In G, TRAM flap migration, showing in the back the rectus abdominis muscle sheaths still not sutured. In H, Plication of the rectus muscles sheath, bilaterally. In I, TRAM flap with its larger axis transversally positioned and the umbilicus hole close to the lower edge of the recipient incision. Details of the normal appearance of the vascularization of TRAM flap's extremities.
Postoperative care
The patients remained hospitalized for 24 to 48 hours and began to walk as soon as the postanesthetic conditions were settled.
The drains were removed after 24 hours, and the patients did not wear elastic girdles like those used in the postoperative period of conventional abdominoplasties.
Strolling was alternated with rest during the first postoperative week, with greater flexibility from the second week on.
Showering was allowed from the second postoperative day, and sports activities, after the second month.
RESULTS
The aesthetic result obtained in all cases was considered satisfactory by the patients and the surgical staff. During the postoperative follow-up, the patients did not develop any type of secondary herniation or bulging in the abdominal wall (Figures 4 to 6).

Figure 4 - Computed tomography scan of an athlete (tennis player), 9 months after the operation.
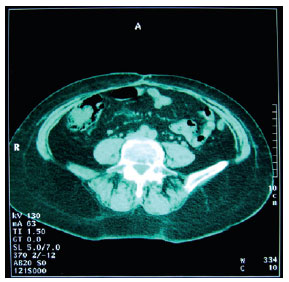
Figure 5 - Computed tomography scan of a patient 9 months after an abdominoplasty using mesh.
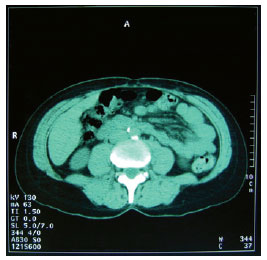
Figure 6 - Computed tomography scan of a patient 10 months after the operation.
In this series of patients, 1 case of seroma, 1 case of fat necrosis, and 1 case of hematoma were observed.
In patients that underwent breast reconstruction, the breast team determined how long drains would remain in (there was one in the axilla and another through the pubis, both connected to the same collector). Drain removal was always linked to a minimum drainage of 100 mL in the last 24 hours.
In patients who underwent late reconstruction, the drains emerged through the pubis, and remained in place for 24 to 48 hours, generally with drainage of 50 to 100 mL in the last 24 hours. The patient with fat necrosis did not have impairment of the dermoepidermal junction, only required local treatment for a period of 30 days, and did not require surgical revision. In the case of the hematoma, it also occurred in the hypogastrium, and surgical drainage was required.
Figures 7 to 11 illustrate the results obtained in the middle and long terms.
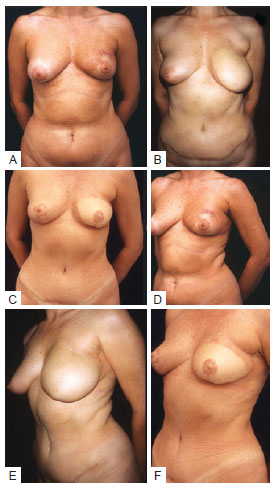
Figure 7 - A 39-year-old patient with a biopsy-confirmed malignant tumor in the left breast, with moderate bulging in the hypogastrium, who underwent mastectomy with immediate reconstruction with TRAM flap. In A, B, and C, Anterior views after the operation, 2 years after the operation, without modeling of the new breast, and 1 year after the second operation, with modeling of the new breast, new areola, and papilla, in addition to homolateral mastopexy. In D, E, and F, Lateral view, showing maintenance of the hypogastrium's normal characteristics without bulging and without the use of mesh.
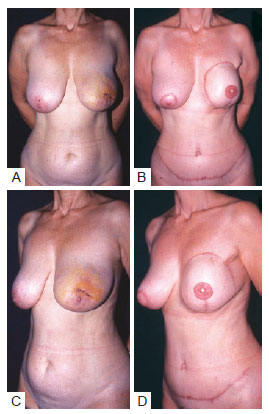
Figure 8 - A 55-year-old patient with hypertrophy and breast ptosis who underwent left mastectomy with immediate reconstruction with bipedicled TRAM flap and treatment of the donor bed without using mesh. In A and B, Anterior preoperative view and anterior view after a second operation for retouching the cutaneous flap, new papilla, and new areola, as well as right mastoplasty for breasts symmetrization, demonstrating the hypogastric conditions without bulging and without using mesh, 8 months after the operation. In C and D, Lateral views in the preoperative period and after the second operation.
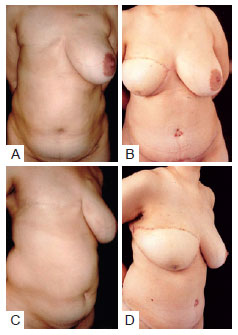
Figure 9 - A 36-year-old patient who underwent right mastectomy 2 years before, via a transverse incision, with partial preservation of the pectoralis muscle close to the axilla. She also had, prior to the surgery, a clear adipose protrusion in the hypogastrium. In A and B, Anterior view before the operation and 6 months after the operation, without abdominal protrusion and without use of mesh. In C and D, Lateral view before the operation and 6 months after the operation.
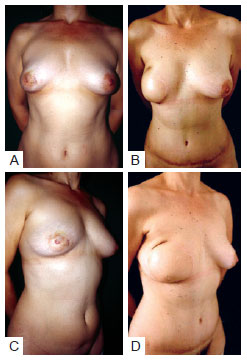
Figure 10 - A 48-year-old patient who underwent right mastectomy and immediate reconstruction with bipedicled TRAM flap without the use of mesh. In A and B, Anterior views before the operation and in the eleventh month after the operation, without retouching of the new breast and demonstrating the hypogastrium without bulging. In C and D, Lateral views in the preoperative period and in the eleventh month after the operation.
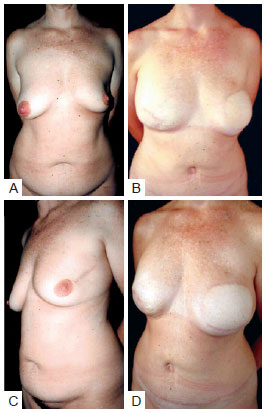
Figure 11 - A 43-year-old patient who underwent left mastectomy and immediate reconstruction with bipedicled TRAM flap. Thirteen months after the radical mastectomy, a subcutaneous mastectomy was performed on the opposite breast, with a prosthetic implant. In A and B, Anterior views of the preoperative appearance and final postoperative appearance 18 months after the mastectomy and reconstruction without retouching of the second operation. Absence of bulging in the hypogastrium, not using mesh. In C and D, Lateral views, before the operation and 18 months after the operation.
DISCUSSION
The purpose of this study is to demonstrate the use of pedicled TRAM flap without the use of mesh for a decreased possibility of herniation in the middle to long term. Therefore, the rectus abdominis muscles should be integrally preserved in the interior of their aponeuroses up to the level of the respective arcuate line, bilaterally.
Many surgeons prefer the single-pedicled TRAM flap as hernia prophylaxis, because of the more complex handling required in the bipedicled TRAM flap in addition to the need for a mesh implant to reinforce the aponeurotic wall. On the other hand, the single-pedicled TRAM flap limits the volume of the flap by up to 50%, by resection of zones IV and part of zone III because of the risk of necrosis (Figures 12 and 13). One, therefore, must take into consideration the limitations of this procedure for reconstructions that require new breasts of greater volume. The bipedicled TRAM flap has the advantage of greater vascularization and greater volume of tissue for the new breast reconstruction.
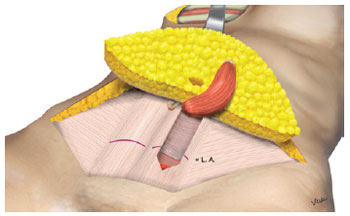
Figure 12 - Illustration of the technique of single-pedicled flap dissection from its aponeurotic sheath, elongating it caudally beyond the arcuate line.
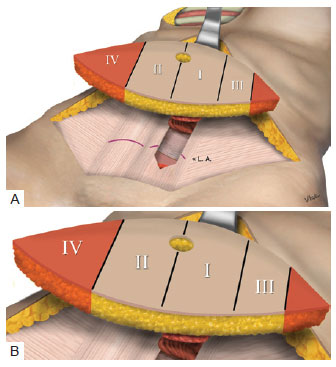
Figure 13 - In A, Schematic detail of the technique usually applied in the single-pedicled flap, in which dissection of the rectus abdominis muscle crosses the arcuate line. In B, Total and partial resection of zones IV and III, respectively, with the purpose of reducing the possibility of necrosis by vascular limitation.
In the literature, authors describing similar procedures do not clearly specify the level where the rectus muscles are sectioned below the arcuate line, only reporting "some centimeters." Therefore, the fragility of the posterior wall of the rectus abdominis muscles sheath explains the presence of secondary bulging and eventrations in the bilateral TRAM flap. The larger the segments of the rectus muscles used as vectors, the greater will be the possibility of the described consequences. The opposite was seen in the patients operated on in this study: the rectus muscles were integrally maintained in their aponeurotic sheaths up to the arcuate line. They are also sutured in the residual aponeurosis of the rectus abdominis muscles, keeping their continuity. This tactic is responsible for the absence of herniations in the operated cases.
The bipedicled flap was systematically used throughout this series of breast reconstruction using TRAM flap. However, in the last 2 years, the use of quilting sutures of the cutaneous abdominal wall was incorporated on the inferior aspect of the respective aponeurosis, effectively reducing the flow of drainage in the immediate postoperative period. However, the use of continuous aspiration drains was maintained, more due to the wide dissection close to the new breast pouch than to the dissected flap. The average length of time for which drains were required ranged between 24 and 48 hours after the operation. In cases of immediate breast reconstruction with TRAM flap, breast surgeons advocate maintenance of the drains for approximately 1 week, due to the wider dissections that include the axilla.
Elastic girdles are not used in order to avoid any extra compression to the muscular pedicles, with possible vascular compromise.
Finally, caution is taken when drawing the final position of the low transverse suture as per the routine with conventional abdominoplasties. This is done to avoid high scars, which can often be seen if they are more than 12 cm from the anterior vulvar commissure, and which limit the use of underwear or swimsuits without their exposure.
CONCLUSIONS
Bipedicled TRAM flap technique with preservation of the rectus abdominis muscles below the arcuate line, without requiring the reinforcement mesh, provides satisfactory results that are maintained in the middle and long term, without development of any type of secondary herniation in the abdominal wall.
REFERENCES
1. Gandolfo EA. Breast reconstruction with a lower abdominal myocutaneous flap. Br J Plast Surg. 1982;35(4):452-7.
2. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69(2):216-25.
3. Drever JM. The lower abdominal transverse rectus abdominis myocutaneous flap for breast reconstruction. Ann Plast Surg. 1983;10(3):179-85.
4. Vasconez LO, Psillakis JM, Johnson-Giebeik R. Breast reconstruction with contralateral rectus abdominis myocutaneous flap. Plast Reconstr Surg. 1983;71(5):668-77.
5. Keppke MK, Pinotti JA, Matta SR. Reconstruções mamárias imediatas. In: Ribeiro L, ed. Cirurgia plástica da mama. Rio de Janeiro: Medsi; 1989.
6. Clugston PA, Gingrass MK, Azurin D, Fisher J, Maxwell GP. Ipsilateral pedicled TRAM flaps: the safer alternative? Plast Reconstr Surg. 2000;105(1):77-82.
7. Erni D, Harder YD. The dissection of the rectus abdominis myocutaneous flap with complete preservation of the anterior rectus sheath. Br J Plast Surg. 2003;56(4):395-400.
8. Kroll SS. Bilateral breast reconstruction in very thin patients with extended free TRAM flaps. Br J Plast Surg. 1998;51(7):535-7.
9. Taylor GI, Corlett RJ, Caddy CM, Zelt RG. An anatomic review of the delay phenomenon: II. Clinical applications. Plast Reconstr Surg. 1992;89(3):408-18.
10. Holmström H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13(3):423-7.
11. Grotting JC, Urist MM, Maddox WA, Vasconez LO. Conventional TRAM-flap versus free microsurgical TRAM-flap for immediate breast reconstruction. Plast Reconstr Surg. 1989;83(5):828-44.
12. Kroll SS, Schusterman MA, Reece GP, Miller MJ, Robb G, Evans G. Abdominal wall strength, bulging and hernia after TRAM flap breast reconstruction. Plast Reconstr Surg. 1995;96(3):616-9.
13. Scheflan M, Dinner MI. The transverse abdominal island flap. Part I: Indications, contraindications, results, and complications. Ann Plast Surg. 1983;10(1):24-35.
14. Boyd JB, Taylor GI, Corlett R. The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast Reconstr Surg. 1984;73(1):1-16.
15. Brown RG, Vasconez LO, Jurkiewicz MJ. Transverse abdominal flaps and the deep epigastric arcade. Plast Reconstr Surg. 1975;55(4):416-21.
16. Miller LB, Bostwick 3rd J, Hartrampf Jr CR, Hester Jr TR, Nahai F. The superiorly based rectus abdominis flap: predicting and enhancing its blood supply based on an anatomic and clinical study. Plast Reconstr Surg. 1988;81(5):713-24.
17. Moon HK, Taylor GI. The vascular anatomy of rectus abdominis musculocutaneous flaps based on the deep superior epigastric system. Plast Reconstr Surg. 1988;82(5):815-32.
18. Rietjens M, Urban CA, De Lorenzi F, Bonato Jr A. Reconstrução mamária com retalho miocutâneo do músculo reto abdominal (TRAM). In: Mélega JM, ed. Cirurgia plástica: fundamentos e arte. Cirurgia reparadora de tronco e membros. Tomo III. Rio de Janeiro: Medsi; 2004.
19. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
Plastic Surgeon of Hospital Santa Edwiges, Full Member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery), Campinas, SP, Brazil.
Eduardo Margy Keppke
Av. Barão de Itapura, 1111
Campinas, SP, Brazil - CEP 13020-432
E-mail: eduardokeppke@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 27, 2012
Article accepted: March 10, 2012
Study conducted at Hospital Santa Edwiges, Campinas, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter