

Original Article - Year 2012 - Volume 27 -
Self-esteem in patients undergoing blepharoplasty
Autoestima em pacientes submetidas a blefaroplastia
ABSTRACT
BACKGROUND: The eyes are important anatomical structures in the aesthetic whole of the face. A person's gaze communicates aspects of their personality and feelings. This study evaluated the effect of blepharoplasty on the patients' self-esteem.
METHODS: From May 2006 to April 2007, 49 female patients aged 30 to 40 years (mean, 34 years) were subjected to blepharoplasty. In the upper eyelids, we excised excess skin and resected excess adipose tissue around the orbit ("fat pockets") in all patients. In 24 and 25 patients, closure with Dermabond® (2-octyl cyanoacrylate) and intradermic suturing with mononylon 6-0, respectively, was performed. In the lower eyelids, we performed lower transconjunctival blepharoplasty without resecting excess skin in 25 patients and lower transconjunctival blepharoplasty with myocutaneous flap in 24 patients. In all the lower eyelids, we resected the excess fat of the adipose body of the orbit. To evaluate the effect of blepharoplasty on the patients' self-esteem, we applied the Rosenberg Self-Esteem Scale before and at 30 and 90 days after the operation. Statistical analyses were performed by applying analysis of variance (ANOVA), Bonferroni correction, and Pearson's linear correlation coefficient.
RESULTS: The mean score in the self-esteem scale changed from 7.0 before the operation to 4.72 and 4.63 after 30 and 90 days of the operation, respectively.
CONCLUSIONS: We observed an improvement in self-esteem after blepharoplasty, but this improvement was only statistically significant in the group subjected to upper blepharoplasty with Dermabond® closure and lower blepharoplasty with myocutaneous flap.
Keywords: Blepharoplasty. Eyelids/surgery. Self concept.
RESUMO
INTRODUÇÃO: Os olhos constituem estruturas anatômicas importantes no conjunto estético da face. O olhar transmite aspectos da personalidade e sentimentos de um indivíduo. O objetivo deste estudo foi avaliar o impacto da blefaroplastia na autoestima das pacientes.
MÉTODO: No período de maio de 2006 a abril de 2007, 49 pacientes do sexo feminino, com idades entre 30 anos e 40 anos, foram submetidas a blefaroplastia. Nas pálpebras superiores, foram realizadas excisão do excedente cutâneo e ressecção do excesso do corpo adiposo da órbita ("bolsas adiposas"), em todas as pacientes. Em 24 pacientes o fechamento foi feito com Dermabond® (2-octil-cianoacrilato) e em 25 foi realizada sutura intradérmica com mononáilon 6-0. Nas pálpebras inferiores, foi realizada blefaroplastia inferior transconjuntival sem ressecção de excedente cutâneo em 25 pacientes, e blefaroplastia inferior transcutânea com retalho miocutâneo em 24. Em todas as pálpebras inferiores foi ressecado o excedente gorduroso do corpo adiposo da órbita. Para avaliar o impacto da blefaroplastia na autoestima das pacientes, foi utilizado o questionário The Rosenberg Self-Esteem Scale, aplicado na fase pré-operatória, um mês e três meses após a cirurgia. A análise estatística foi feita pela análise de variâncias com medidas repetidas (ANOVA), complementada pelo método de Bonferroni. Foi empregado o coeficiente de correlação linear de Pearson. A média de idade foi de 34 anos.
RESULTADOS: O escore médio da escala de autoestima passou de 7, no pré-operatório, para 4,72 no primeiro mês e 4,63 no terceiro mês de pós-operatório.
CONCLUSÕES: Foi observada melhora da autoestima nas pacientes submetidas a blefaroplastia, melhora estatisticamente significante apenas nos grupos submetidos a blefaroplastia superior com fechamento com Dermabond e inferior com retalho miocutâneo.
Palavras-chave: Blefaroplastia. Pálpebras/cirurgia. Auto-imagem.
The eyes are probably the most important aesthetic unit of the human body. When areas surrounding the eyes appear fresh and shiny, the person appears to have an aura of health, vitality, and youth. The opposite is observed when a person's eyes look tired, sad, or aged1.
The ocular region is the central aesthetic unit of the face. One look may privately communicate aspects of individual personality and feelings, which may change with aging. Assuming this, the orbitopalpebral region plays an important role, complementing this form of expression1,2.
Age-related changes are noticeable primarily around the eyes. Nowadays, there are several techniques, based on different principles, to correct age-related deformities that appear in the eyelid3. Fortunately, the eye area offers better opportunities for aesthetic improvements than any other part of the face or perhaps the entire body1.
Blepharoplasty (Greek: blepharos refers to the eyelids and plastikós refers to shape) is the surgery aimed at eyelid rejuvenation. This surgery may be performed alone or in combination with other procedures aimed at treating signs of aging2-5.
In 1844, Sichel was the first to discuss the treatment of sagginess and excess tissue in the eyelids. In 1896, Fuchs described excision to correct blepharochalasis. However, eyelid surgeries only took off in 1951 with standardization of the basic principles of the technique according to the various anatomical structures, which were elaborated on by Castañares1,2,6,7.
The classical techniques of blepharoplasty aim to improve and correct the function, shape, and aesthetic appearance of the eyelids. This procedure is certainly among the most performed procedures in plastic surgery. Blepharoplasty normally yields good results. However, despite its apparent simplicity, there is great and varied potential for complications8.
The primary aim of lower blepharoplasty is eyelid rejuvenation, which is almost always accomplished by adequate resection of the adipose body of the orbit (i.e., adipose pockets) and cutaneous treatment when needed. There are 2 approaches to treat the lower eyelids. The first is the transcutaneous approach in which the skin, muscle, and adipose bodies are removed via an infraciliary cutaneous incision. This approach offers excellent exposure of the adipose body and an acceptable final scar. However, large numbers of complications can occur, including scleral show and ectropion gravis9,10. The incidence of lower eyelid retraction after transcutaneous blepharoplasty is approximately 20%11,12.
The second approach is the transconjunctival approach, which was initially described by Bourget in 1924; it is widely accepted nowadays due to its low incidence of complications11-13. Five decades later, Tessier popularized this approach for the treatment of congenital malformations of the eyelid14. This technique gained widespread popularity after Zarem and Resnick15 reported that it avoids complications associated with transcutaneous blepharoplasty with myocutaneous flap. It is generally indicated in young patients or patients with redundant adipose bodies of the orbit with little or no excess skin13. The transconjunctival approach does not produce visible scars and allows direct treatment of the adipose body of the orbit without damaging the skin, orbicular muscle, or orbital septum. Recently, many authors started to defend the use of lower transconjunctival blepharoplasty for older patients with some degree of skin redundancy and sagginess of the muscle and ligaments. The major limitation of this procedure is the treatment of excess skin, which requires additional procedures such as peelings, laser treatment, or even surgical skin resection3-5,16.
Alternatives to conventional sutures have been researched for more than 30 years. Although cyanoacrylate, a tissue adhesive polymer, existed since 1919, it was only after the development of butyl-2-cyanoacrylate (Histoacryl: B. Brown Medical Inc., Sheffield, England) in the 1970s that adhesives and tissue glues started to be used for closing wounds17. This prompted several studies to focus on reducing surgical time, inducing fast wound healing, and increasing patient comfort17-19.
Toriumi and Bagel19 report the use of tissue adhesives in cases of blepharoplasties and even tissue lacerations without observing significant adverse clinical effects.
In 1998, the American Food and Drug Administration (FDA) approved the use of octyl-2-cyanoacrylate (Dermabond; Ethicon, Johnson & Johnson, New Brunswick, NJ, USA) for the closure of wounds and as a bacterial barrier. This new generation of cyanoacrylates exhibits better flexibility and closure effectiveness in addition to reduced histotoxicity and better bactericidal action18.
Plastic surgery has been directed towards final acceptable aesthetic results and a postoperative period free of complications. However, for patients, eyelid correction has much broader implications, involving several aspects of their lives20.
The evaluation of medical procedures is traditionally based on objective evaluation measures such as mortality and morbidity. Medical judgment on treatment efficacy is made using parameters such as clinical, laboratory, and radiological evaluations21. In an attempt to generalize the evaluation of results of clinical or surgical treatments, the concept of quality of life has been used in several areas of medical care. Some instruments for evaluating the quality of life associated with health have been proposed. The quantification of quality of life is important in plastic surgery considering that the conditions treated not only have physical implications, but strong social, psychological, and emotional implications as well21,22.
The World Health Organization (WHO, Geneva, 1958) established the concept of health as not only the absence of disease, but also a complete state of physical, psychological, and social wellbeing; this definition resembles the concept of quality of life. The perception of quality of life differs from person to person, and there are 2 categories of instruments for evaluating quality of life: generic and specific.
Generic instruments can be applied to a large variety of populations since they include aspects related to function, dysfunction, and physical and emotional discomfort, which are relevant to the quality of life. The repeated use of these instruments during a period of time may define improvement or worsening of the physical and emotional aspects of patients, making them useful for evaluating the results obtained by certain interventions23.
Specific instruments are capable of evaluating certain aspects of the quality of life in specific ways, providing greater capacity to detect improvement or worsening of the aspect in question. Their main characteristic is their potential to be sensitive to changes after intervention. They may be specific to certain functions (e.g., physical capabilities, sleep, and sexual function), populations (e.g., old and young), or changes (e.g., pain)24.
The Rosenberg Self-Esteem Scale is used in Brazilian studies because it is already available in Portuguese and its measurement properties such as reproducibility, validity, and responsiveness have already been demonstrated. The Rosenberg Self-Esteem Scale is a specific instrument with psychometric properties for self-esteem only25.
Self-esteem can be defined as the feeling of appreciation and consideration a person feels for himself or herself being the center of their subjective life, which in turn determines their thoughts and behavior. In this way, self-esteem can be analyzed and quantified objectively on the basis of social experiences26,27.
The idea that a patient's perception of his/her own health should be considered when evaluating the effectiveness of a medical treatment is becoming increasingly accepted, particularly in plastic surgery where the psychological component is important for the evaluation of postoperative results.
This study aims to evaluate the relationships between self-esteem and upper blepharoplasty with or without 2-octyl-cyanoacrylate (Dermabond®) and lower transconjunctival blepharoplasty with or without myocutaneous flap.
METHODS
From May 2006 to April 2007, a prospective study was performed with 49 patients subjected to blepharoplasty. The inclusion criteria for the study were as follows: female patients, Caucasian or Asian, 30-40 years of age, excess skin on the upper eyelids, obvious adipose pockets (i.e., in the adipose body of the orbit), and little excess skin on the lower eyelids.
The exclusion criteria for the study were as follows: tobacco use; acute, relapsing, or chronic diseases; patients taking daily medication; previous treatment of the eyelid area; sensitivity to lidocaine or 2-octyl-cyanoacrylate; and illiteracy. A minimum of basic schooling was required.
All patients freely signed informed consent forms prior to participation.
Surgical technique
All patients were subjected to upper and lower blepharoplasty under local anesthesia and sedation in a hospital environment. For the local anesthetic, we used 2% lidocaine with 1:200,000 diluted vasoconstrictor freshly prepared at the time of surgery. In all upper blepharoplasties, the excess skin and adipose body of the orbit were removed (Figure 1). All patients were divided into 4 groups during surgery. This division was done stochastically by lottery:

Figure 1 - Marking of excess skin to be resected.
Group I: Upper blepharoplasty and closure with intradermic mononylon 6-0 sutures. Lower blepharoplasty with transcutaneous infraciliary incision, detachment of the myocutaneous flap, and resection of the excess skin and adipose body of the orbit. Group II: Upper blepharoplasty and closure with 2-octyl-cyanoacrylate (Dermabond®). Lower blepharoplasty with transcutaneous infraciliary incision, detachment of the myocutaneous flap, and resection of the excess skin and adipose body of the orbit (Figure 2).

Figure 2 - Patient in group II (use of Dermabond® in the upper eyelids) 7 days after the operation.
Group III: Upper blepharoplasty and closure with intradermic mononylon 6-0 sutures. Lower transconjunctival blepharoplasty with resection of the excess adipose body of the orbit (Figure 3).

Figure 3 - Transconjunctival approach exposing the adipose body of the orbit.
Group IV: Upper blepharoplasty and closure with 2-octyl-cyanoacrylate (Dermabond®).
Patients were discharged from the hospital 6 to 12 hours after the completion of the surgery. First-generation cephalosporin (i.e., cephalexin; 500 mg) was prescribed every 6 hours for 7 days; sodium dipyrone, 35 drops every 6 hours when needed to manage pain; lubricant collyrium, 2 drops in each eye 6 times a day for 7 days; and night ophthalmic ointment before sleep for 7 days. Furthermore, patients were instructed to apply cold compresses on the eyes with a gel mask every 2 hours in the first 3 postoperative days and lie down with the upper body elevated for 7 days. The sutures were removed 4 days after the operation.
Postoperative evaluations
Postoperative evaluations were carried out during consultation by the same investigator who conducted the preoperative phase on postoperative days 4, 7, 14, 30, 60, and 90; this included clinical evaluation, photographic documentation, and a self-esteem questionnaire (at the 1st and 3rd months).
Self-esteem instrument
We used the Brazilian version of the Rosenberg Self-Esteem Scale questionnaire to evaluate possible changes in the patient's self-esteem caused by blepharoplasty. The Rosenberg Self-Esteem Scale questionnaire was translated and validated for the Brazilian cultural context by Dini27. It is a simple, quick, easy to understand, and widely used questionnaire in the medicine literature. This questionnaire is a specific instrument for measuring the quality of life; it is composed of 10 multiple-choice questions with 4 options each exclusively about self-esteem26. The patient can only choose one answer for each question according to what they feel at that moment. Each answer is scored from 0-3; the total score is calculated by adding the scores of the 10 questions. The total score ranges from 0-30, with 0 and 30 representing the best and worst states of self-esteem, respectively.
Statistical analyses
A descriptive scale was used to analyze the demographic results. The means (M) and standard deviations (SD) were calculated for numerical variables, and frequency (%) was calculated for categorical variables.
Statistical analyses were performed by analysis of variance (ANOVA) with a Bonferroni correction. We also calculated Pearson's linear correlation coefficients. P < 0.05 was considered statistically significant.
RESULTS
Patients completed all stages of the postoperative period.
The patients were divided into 4 groups by using a lottery system at the time of surgery. Groups I, II, and IV included 12 (24.5%) patients each, while group III had 13 (26.5%).
No patient required emergency surgical procedures due to complications such as hematomas, seromas, necrosis, or dehiscences. Only 1 (2.05%) patient in group II developed discreet ectropion in the right lower eyelid that spontaneously regressed by 30 and 90 days after the operation.
Rosenberg self-esteem scale results
All patients responded to the questionnaire before and at 30 and 90 days after the operation. The mean preoperative and 30-day postoperative scores of all groups were 7.0 ± 3.49 and 4.72 ± 3.24, respectively, showing improved self-esteem in all groups. Ninety days after the operation, the mean score was 4.63 ± 3.52, indicating the maintenance of self-esteem compared to 30 days after the operation, but improvement compared to that before surgery (Figure 4).
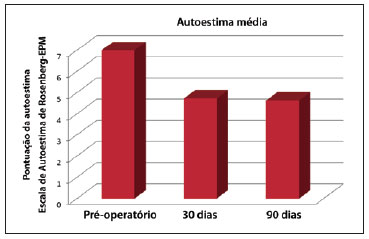
Figure 4 - Mean self-esteem scores of the patients before and at 30 and 90 days after the operation.
Examining the 4 groups separately, the mean preoperative, and 30- and 90-day postoperative scores of group I were 5.3 ± 4.9, 4.1 ± 4.0, and 5.1 ± 4.0, respectively (P = 0.397); group II were 6.8 ± 3.7, 3.5 ± 2.7, and 3.2 ± 3.7, respectively (P = 0.005); group III were 7.6 ± 6.3, 6.1 ± 5.4, and 5.9 ± 5.0, respectively (P = 0.490); and group IV were 6.3 ± 3.2, 7.2 ± 4.4, and 4.8 ± 4.5, respectively (P = 0.069).
All study groups exhibited improvements in the mean self-esteem score. However, the improvement was only statistically significant in group II (P < 0.05).
DISCUSSION
There is no consensus on the ideal approach for plastic surgeries of the lower eyelids. Each plastic surgeon develops his/her preference. The evolution of lower blepharoplasty is the result of different concepts. Some authors favor maintaining adipose pockets, some are against manipulating the orbicular muscles, and others recommend ample detachment of the myocutaneous flap. However, these principles cannot be applied to all patients. Each approach must be individualized, aiming to achieve the best results with the lowest risk of complications28.
Transconjunctival access has become popular in the last decade, and its list of indications has expanded. Meanwhile, the transcutaneous approach remains the first choice in some situations. Although some procedures that aim to resect and retract excess skin have been described in association with transconjunctival blepharoplasty, most surgeons still prefer the transcutaneous approach when there is excess skin in the lower eyelid. In patients with orbicular muscle hypertrophy who require muscular excision, the best treatment is achieved through the transcutaneous approach and detachment of the myocutaneous flap29,30.
The transconjunctival approach to the lower eyelid is an excellent method for decreasing the volume of adipose pockets and maintaining the position and contour of the lower eyelids. Meanwhile, transcutaneous lower blepharoplasty produces a visible external scar and can result in changes in the margin and contour of the lower eyelid as complications. Lower transconjunctival blepharoplasty offers a significantly lower risk of retraction of the lower eyelids3,9,10,28.
Patients subjected to lower transconjunctival blepharoplasty who have excess skin may benefit from alternative treatments such as laser resurfacing or chemical peeling, or have skin resection via the transconjunctival approach3-5.
Octyl-2-cyanoacrylate (Dermabond®) was initially used in pediatric patients with small traumatic lacerations that needed sutures. However, many trauma surgeons started to use this procedure because it eliminated the need to remove sutures and showed good aesthetic results. Several studies in plastic surgery involve the use of 2-octyl-cyanoacrylate in blepharoplasties and mammoplasties18,19.
The Rosenberg Self-Esteem Scale is a specific instrument with psychometric properties that measures the patient's self-esteem at the time they answer the questionnaire25. It is an objective way to quantify the results of a procedure that does not depend on subjective or examiner-dependent evaluations.
Despite the diverse currently used blepharoplasty techniques and most modern options for wound closure found in the literature, we observed that plastic surgery in general plays a very important role in the patients' self-esteem. Regardless of the technique used, we observed improved self-esteem in all study groups.
The statistically significant improvement in self-esteem in group II in our study further confirms the effect of blepharoplasty on the lives and self-esteem of those patients.
CONCLUSIONS
We observed improvement in the self-esteem of patients subjected to blepharoplasty. However, this improvement was statistically significant only in the group subjected to upper blepharoplasty and closure with 2-octyl-cyanoacrylate (Dermabond®) and to lower blepharoplasty with transcutaneous infraciliary incision and myocutaneous flap.
REFERENCES
1. Flowers RS, Duval C. Blepharoplasty and periorbital aesthetic surgery. In: Aston SJ, Beasley RW, Thorne CHM, eds. Grabb and Smith's Plastic Surgery. 5th ed. Philadelphia: Lippincott-Raven Publishers; 1997. p. 609-32.
2. Moelleken B. The superficial subciliary cheek lift, a technique for rejuvenating the infraorbital region and nasojugal groove: clinical series of 71 patients. Plast Reconstr Surg. 1999;104(6):1863-76.
3. Shore N. Lower lid transconjunctival blepharoplasty using the CO2 laser. Aesthetic Surg Q. 1996;101.
4. Seckel BR, Kovanda CJ, Cetrulo CL Jr, Passmore AK, Meneses PG, White T. Laser blepharoplasty with transconjunctival orbicularis muscle/septum tightening and periocular skin resurfacing: a safe and advantageous technique. Plast Reconstr Surg. 2000;106(5):1127-45.
5. Rosenfield L. Pinch blepharoplasty: a safe technique with superior results. Aesthet Surg J. 2007;27(2):199-203.
6. Millman AL, Williams JD, Romo T 3rd, Taggert N. Septal-myocutaneous flap technique for lower lid blepharoplasty. Ophthal Plast Reconstr Surg. 1997;13(2):84-9.
7. Castañares S. Blepharoplasty for herniated infraorbital fat: anatomical basis for a new approach. Plast Reconstr Surg. 1951;8(1):46-58.
8. Jaimovich CA, Medeiros R. Blefaroplastia convencional. In: Mélega JM, ed. Cirurgia Plástica: fundamentos e arte. Cirurgia estética. Rio de Janeiro: Medsi; 2003. p. 105-16.
9. Lessa S. Blefaroplastia não-convencional. In: Mélega JM, ed. Cirurgia Plástica: fundamentos e arte. Cirurgia estética. Rio de Janeiro: Medsi; 2003. p. 117-29.
10. Baylis HI, Long JA, Groth MJ. Transconjunctival lower eyelid blepharoplasty: technique and complications. Ophthalmology. 1989;96(7):1027-31.
11. McGraw BL, Adamson PA. Postblepharoplasty ectropion: prevention and management. Arch Otolaryngol Head Neck Surg. 1991;117(8):852-6.
12. Lessa SF, Elena EH, Araújo MRC, Pitanguy I. Modificações anatômicas da fenda palpebral após blefaroplastia. Rev Bras Cir. 1997;87(4):179-88.
13. Whitaker LA. Selective alteration of palpebral fissure form by lateral canthopexy. Plast Reconstr Surg. 1984;74(5):611-9.
14. Tessier P. The conjunctival approach to the orbital floor and maxilla in congenital malformation and trauma. J Maxillofac Surg. 1973;1(1):1-8.
15. Zarem HA, Resnick JI. Expanded applications of transconjunctival lower lid blepharoplasty. Plast Reconstr Surg. 1991;88(2):215-20.
16. Campbell G. Tips to prevent complications with transconjunctival blepharoplasty. Aesthet Surg J. 1997;17(6):388-9.
17. Kramer FM, Joseph JH. Histoacryl: its use in aesthetic facial plastic surgery. Arch Otolaryngol Head Neck Surg. 1989;115(2):193-7.
18. Perin LF, Helene Jr A, Fraga MF. Sutureless closure of the upper eyelids in blepharoplasty: use of octyl-2-cyanoacrylate. Aesthet Surg J. 2009; 29(2):87-92.
19. Toriumi DM, Bagel AA. Cyanoacrylate tissue adhesives for skin closure in the outpatient setting. Otolaryngol Clin North Am. 2002;35(1):103-18.
20. Ferreira LM, Hochman B. Blefaroplastia. In: Ferreira LM, ed. Guia de Cirurgia Plástica. Barueri: Manole; 2007. p. 649-55.
21. Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622-9.
22. Rankin M, Borah GL, Perry AW, Wey PD. Quality-of-life outcomes after cosmetic surgery. Plast Reconstr Surg. 1998;102(6):2139-47.
23. Ebrahim S. Clinical and public health perspectives and applications of health-related quality of life measurement. Soc Sci Med. 1995;41(10):1383-94.
24. Guyatt GH. A taxonomy of health status instruments. J Rheumatol. 1995;22(6):1188-90.
25. Shakespeare V, Cole RP. Measuring patient-based outcomes in a plastic surgery service: breast reduction surgical patients. Br J Plast Surg. 1997;50(4):242-8.
26. Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965. 326 p.
27. Dini G. Validação e adaptação cultural da versão brasileira da escala de autoestima de Rosenberg [dissertação de mestrado]. São Paulo: Escola Paulista de Medicina - UNIFESP/EPM; 2000.
28. Castro CC. A critical analysis of the current surgical concepts for lower blepharoplasty. Plast Reconstr Surg. 2004;114(3):785-96.
29. Adamson PA, Strecker HD. Transcutaneous lower blepharoplasty. Facial Plast Surg. 1996;12(2):171-83.
30. Jacono AA, Moskowitz B. Transconjunctival versus transcutaneous approach in upper and lower blepharoplasty. Facial Plast Surg. 2001;17(1):21-8.
Plastic Surgeon, Full Member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society for Plastic Surgery), coordinator of the Plastic Surgery team of the Hospital Estadual de Diadema, Diadema, SP, Brazil; coordinator of the Plastic Surgery League of the Universidade Federal de São Paulo (Federal University of São Paulo) - Unifesp, doctor of the section of health insurance of the Disciplina de Cirurgia Plástica - UNIFESP/ Hospital São Paulo, São Paulo, SP, Brazil.
Carlos Koji Ishizuka
Rua Borges Lagoa, 783 - cjto. 42 - Vila Clementino
São Paulo, SP, Brazil - CEP 04038-031
E-mail: kojiishizuka@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: May 28, 2011
Article accepted: November 11, 2011
Study conducted at the private clinic of the author, São Paulo, SP, Brazil.
This study was presented to aid promotion to a Full Member of SBCP.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter