

Original Article - Year 2012 - Volume 27 -
Assessment of nasal anthropometric parameters after primary cleft lip repair using the Mohler technique
Avaliação de parâmetros antropométricos nasais após queiloplastia primária pela técnica de Mohler
ABSTRACT
BACKGROUND: Efforts to obtain the best possible results in the nasal region of cleft patients are an ongoing process; it is therefore essential to correctly diagnose any changes in the nasal anatomy of cleft palate patients that occur over time and after surgical intervention. The aims of the present study were: (1) to evaluate the percentage of nose asymmetry in patients with either complete or incomplete unilateral cleft lip and palate who underwent primary cleft lip repair with the Mohler technique, both in the immediate postoperative period (T1) and after 1 year (T2); and (2) to compare the percentage of nasal asymmetry in both postoperative periods using the same indexes in children without cleft lip and palate.
METHODS: During the period from March 2007 to December 2010, 27 patients with unilateral cleft lip and palate were submitted to primary cleft lip repair. Measurements of area, height, height at ¼ of the medial width, and height of the base of the nose were obtained from two-dimensional photos by using Adobe Photoshop CS5 Extended®. Statistical comparison of the values obtained for nasal asymmetry in the immediate postoperative period and 1 year after surgery was performed with ANOVA.
RESULTS: Percentile indexes of nasal asymmetry for cleft patients showed statistical differences in all variables when compared to controls, with the exception being the base of the nose.
CONCLUSIONS: The results we obtained showed an improvement in nasal symmetry, although there was a tendency to relapse from the result obtained in T1. Patients with complete cleft were more susceptible to relapse with regard to the position of the nose.
Keywords: Cleft palate. Cleft lip. Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Os esforços para obtenção de melhores resultados da região nasal de pacientes fissurados são contínuos, portanto é necessário o correto diagnóstico das alterações da anatomia nasal sofrida com o decorrer do tempo após uma intervenção cirúrgica. Os objetivos do presente estudo foram: 1) avaliar o porcentual de assimetria do nariz de pacientes portadores de fissura labiopalatina unilateral completa e incompleta submetidos a queiloplastia primária com a técnica de Mohler, no pós-operatório imediato (T1) e após um ano da cirurgia (T2); e 2) comparar o porcentual de assimetria nasal em ambos os períodos pós-operatórios com os mesmos índices obtidos em crianças não-portadoras de fissura labiopalatina.
MÉTODO: No período de março de 2007 a dezembro de 2010, 27 pacientes portadores de fissura labiopalatina unilateral foram submetidos a queiloplastia primária. Foram obtidas medidas de área, altura, largura, altura em ¼ medial da largura e altura da base narinar identificados na fotografia em duas dimensões por meio do programa Adobe Photoshop CS5 Extended®. Foi utilizado o teste de ANOVA para comparação estatística entre os valores da assimetria nasal no pós-operatório imediato e um ano após a cirurgia.
RESULTADOS: Foram obtidos índices porcentuais de assimetria nasal entre os pacientes fissurados e o grupo controle, demonstrando diferença estatística em todas as variáveis quando comparado ao grupo controle, exceto quanto à altura da base narinar.
CONCLUSÕES: Os resultados obtidos demonstraram melhora da simetria nasal, porém tendência a recidiva do resultado obtido em T1. Os pacientes com fissura completa são mais suscetíveis à recidiva em relação à posição do nariz.
Palavras-chave: Fissura palatina. Fenda labial. Procedimentos cirúrgicos reconstrutivos.
The first surgical attempts to correct cleft lip and palate date from 390 CE, in China, and were accomplished by joining the two extremities of the lip gap1. In 1956, Lemos2 published the technique for correction of cleft lip by means of Z-plasty. Spina and Lodovici3 and Spina et al.4 made important contributions to the treatment of cleft patients. Spina et al.4 developed one of the most common classification systems for cleft lip and palate in Brazil, as well as the technique for primary cleft lip repair with triangular flaps.
An important event in the field took place in 1955, during the International Congress of Plastic Surgery in Stockholm, when Ralph Millard presented his data on the technique of rotation/advancement5. This technique was subsequently adopted and modified by several surgeons.
In 1972, Mohler described a variation of the technique created by Millard, in which he used a columellar flap (C-flap) that was smaller than the one initially used by Millard and extended the incision vertically by 2 mm, thereby allowing for more columellar extension6-8.
In 1975, McComb9 published an article emphasizing the need for primary rhinoplasty during cleft lip repair by suturing the alar cartilages at a higher anatomical point than the triangular cartilage and thus providing overcorrection of the anatomical structures. Nowadays, surgeons who work with cleft patients increasingly agree on the importance of primary rhinoplasty during cleft lip repair.
Cutting10, Wong et al.11, and Mulliken and Martínez-Pérez12 proposed technical modifications of primary rhinoplasties that provided significant improvement in the nasal symmetry of cleft patients. Cutting10 intensified the work on the nasal area, altered the traction sutures of McComb9, and transformed them into percutaneous sutures with the knot fixed in the internal region of the nose. This maneuver avoids scarring on the child's skin and the sutures have the same effectiveness as traction sutures. Wong et al.11 completely loosened the entire region of the alar cartilages, replaced it in a more appropriate anatomical region, and, afterward, included a resorbable internal splint in the nose that prevents relapse of the nasal deformity.
Efforts are always being made to obtain better results on cleft patients' noses; it is therefore necessary to correctly diagnose the changes in nasal anatomy that occur with time after a surgical intervention.
The present work aims at evaluating the percentage of nasal asymmetry in patients with unilateral complete or incomplete cleft lip and palate subjected to primary cleft lip repair through the Mohler technique, both in the immediate postoperative period (T1) and 1 year after surgery (T2). Also, this study compared the percentage of nasal asymmetry found at both postoperative periods (T1 and T2) with the same indexes in children without cleft lip and palate.
METHODS
We selected 27 patients with ages ranging from 3 to 6 months, of whom 6 had an incomplete cleft and 21 had a complete cleft; the mean age was 4.66 months at T1 (immediate postoperative) and 25.55 months at T2 (> 1 year post surgery). All patients were operated on by the same surgeon (CERA) during the period from March 2007 to December 2010, and underwent primary cleft lip repair using the Mohler technique.
The surgery was performed under general anesthesia. The endotracheal tube was fixed centrally over the lower lip to avoid distortions in the upper lip. Local anesthesia was then applied with 2 mL lidocaine in the nasal and maxillary region. The upper lip was not infiltrated, to avoid distortion of the vermilion border of the lip.
Preoperative marking was performed with methylene blue. A magnifying glass was used for more precise marking.
The lower point of the Cupid's bow was labeled point 1. Point 2 corresponded to the philtral column of the noncleft side and point 3 to replication of the distance 1-2. For a 4-month old patient, the ideal distance between points 1 and 2 is 3 mm, therefore forming a Cupid's bow measuring 6 mm (the distance between points 2 and 3). Point 4 was the most important in the preoperative marking. This point was identified in the region of more cutaneous pigment of the white line, normally 1 mm medially to the point promoted by Cutting; in this way, a smaller quantity of tissue is lost. Point 5 was marked in the region of the cleft nasal wing, approximately 1 mm from the beginning of the nose. Point 6 was marked in the region of the noncleft nasal wing.
According to Cutting10, the distance between points 4 and 5 should be the same as the distance between points 6 and 2. When retracting the cleft nostril with a double hook, point 4 was observed to move from 1 to 2 mm; for that reason, point 4 was marked in the region of more cutaneous pigmentation of the white line. The distance between points 4 and 5 was reproduced for points 4 and 7 inside the gingiva, at the base of the pyriform aperture. Point 7 was the reference region of the base of the lateral flap, also known as the L-flap. Point 8 was drawn on the base of the columella.
After marking, the distances between the points were measured and documented in the patient report. The union of points 3 and 8 and of point 3 with the entrance of the nose formed the columellar flap (C-flap), which was used to elongate the columella on the cleft side. Union of points 4 and 7 and of points 4 and 5 formed the lateral flap (L-flap). The lateral tissue remaining after creating the C-flap formed the mucous flap (M-flap). The points marked were tattooed with methylene blue and a thin needle (Figures 1 and 2).
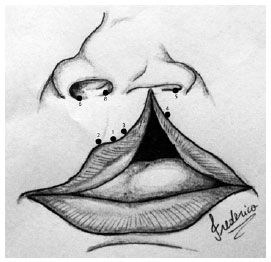
Figure 1 - Illustrative drawing showing the marking points.
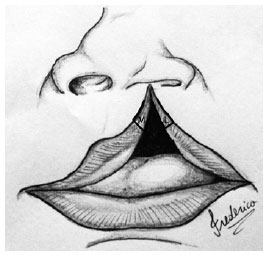
Figure 2 - Illustrative drawing showing the L-flap (lateral) and M-flap (mucosa).
The nasal region was initially released through a columellar incision and amplified by the lateral incision used for making the L-flap. The alar cartilage was thoroughly dissected and repositioned by means of the percutaneous points in a more anatomical region. These same points were used to generate the nasal grooves. After this correction, silicone stents were inserted in the nasal cavities, to support the nasal structures. For comparison, 50 children without cleft lip and palate, aged 10 months to 4 years (mean 38.28 months), were defined as the control group.
All patients and children in the control group had release forms signed by their legal representatives and the study was approved by the Ethical Committee of the SOBRAPAR Craniofacial Surgery Institute (Campinas, SP, Brazil).
The measurements of the nose were obtained through postoperative photos taken in the nasoglabellar position, using as reference the anthropometric scale and measurements of the columella that were obtained in the intraoperative period with the aid of a surgical compass. Photos of the patients were therefore analyzed at two time points: T1, immediate postoperative; and T2, 1 year postoperatively.
The photos of the children from the control group were analyzed in one sitting. Using the program Adobe Photoshop CS5 Extended®, the nose area, nose height, nose width, height at ¼ of the medial width, and the height of the base of the nose13 were calculated on the cleft and noncleft sides (Figure 3).
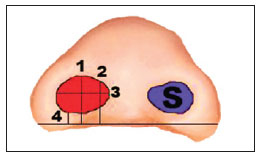
Figure 3 - Schematic drawing illustrating the analyzed anthropometric measurements: 1 = nose height; 2 = height at ¼ of the medial width; 3 = nose width; 4 = height of the base of the nose. S = nose area.
Initially, using the above mentioned program, the columellar height was obtained in pixels; next, that measure in pixels was correlated with the real measurement in millimeters that was obtained using a compass during the surgery, resulting in the length in millimeters. The nose area was then calculated based on the above-cited correlation. In this way, an exact value in mm2 was obtained.
A straight line was drawn between the most medial points of the lateral edges of the nostrils, on both the cleft and noncleft sides; in a similar manner, the highest nose height, the largest width, the height at ¼ of the medial width, and the height of the nose base13 were measured. The measurements of the cleft side, in millimeters, were S1 (nose area), A1 (nose height), L1 (nose width), Alt 1 ¼ (height at ¼ of the medial width), and AB1 (height of the base of the nose). On the noncleft side, the measurements were named in the same way, using the number 2, and the formula proposed by Mulliken and Martínez-Pérez12 was applied, with I being in this case, the asymmetry index for the nose area.
As far as the other measurements are concerned, only the relationships between them were calculated. In the control group, the same measurements were performed and the same formulas and ratios were applied; however, the greater values (of area, height, width, height at ¼ of the medial nose width, and height of the base of the nose, between the nostrils) were given the number 1 (e.g., S1, A1, L1, etc.), while the measurements of lesser value were given the number 2, therefore determining the asymmetry index.
The mathematical equation described by Mulliken allowed the calculation of asymmetry, as a percentage, between the contours of the alar cartilages of the cleft and noncleft sides in the postoperative period and between the larger and smaller sides for the control group11.
The results obtained were then submitted to mathematical analysis using ANOVA, which compared the nasal asymmetry indexes of the patients with incomplete cleft and complete cleft at the aforementioned two time points with the indexes for the control group.
RESULTS
The mean asymmetry index of the nose area was 16.49 ± 11.15% in the immediate postoperative period (T1), and 9.62 ± 9.29% at T2 (>1 year post surgery). For the patients with complete cleft, this index was 17.7 ± 12.08% at T1 and 11.77 ± 9.49% at T2. For the patients with incomplete cleft, the index of asymmetry for the nose area was 14.48 ± 7.52% at T1 and 2.09 ± 1.35% at T2. The control group had a value of 7.24 ± 6.25%. A statistically significant difference compared to the control group was observed at T1 for the patients with complete cleft and also for the group constituted by all patients pooled together (P < 0.001) (Figure 4).
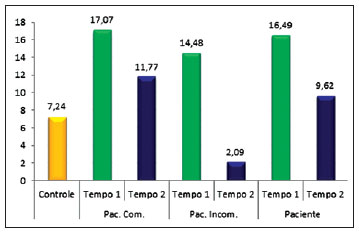
Figure 4 - Graph comparing nasal area between the control group and patients with complete cleft (Pat. Comp.), with incomplete cleft (Pat. Incomp.), and all patients pooled into a single group (Patient).
The mean relationship of the nose height for all patients was 0.96 ± 0.16 at T1 and 0.84 ± 0.12 at T2. For the patients with complete cleft, this relationship was 0.95 ± 0.16 at T1 and 0.84 ± 0.12 at T2. Concerning the patients with incomplete cleft, the relationship was 0.94 ± 0.16 at T1 and 0.84 ± 0.11 at T2. The control group had a mean value of 1 ± 0.07. There was a statistical difference (P < 0.001) at T2 for the group of patients with complete and incomplete cleft, as well as for the group formed by the entire pool of patients (Figure 5).
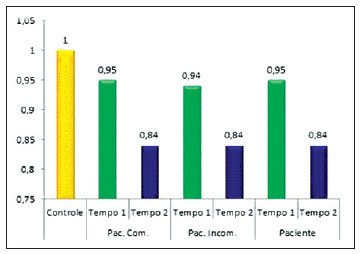
Figure 5 - Graph comparing nose height between the control group and patients with complete cleft (Pat. Comp.), with incomplete cleft (Pat. Incomp.), and all patients pooled into a single group (Patient).
With regard to the width, the patients showed a relationship of 1.02 ± 0.21 at T1, and 1.21 ± 0.28 at T2 (Figure 6). Individually, the patients with complete cleft showed a relationship of 1.04 ± 0.2 at T1 and 1.25 ± 0.27 at T2. The patients with incomplete cleft showed a relationship of 0.95 ± 0.22 at T1 and 1.07 ± 0.28 at T2. The control group showed a relationship of 1.03 ± 0.07. There was a statistical difference in nose width at T2 between patients and controls, with P = 0.006 for the patients with complete cleft and 0.003 for the group formed by the entire pool of patients.
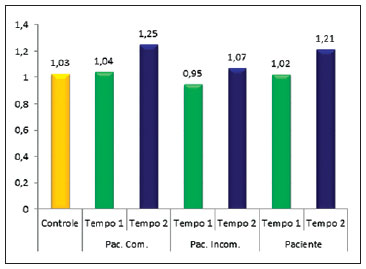
Figure 6 - Graph comparing nose width between the control group and patients with complete cleft (Pat. Comp.), with incomplete cleft (Pat. Incomp.), and all patients pooled into a single group (Patient).
For the ratio between the height at ¼ of the medial width and the nose width, the patients had a value of 1.02 ± 0.26 at T1 and 0.82 ± 0.11 at T2. Individually, for the patients with complete cleft, the relationship was 1.04 ± 0.28 at T1 and 0.82 ± 0.12 at T2. For the patients with incomplete cleft, the relationship was 0.96 ± 0.15 at T1 and 0.86 ± 0.11 at T2. In the control group, the relationship was 0.97 ± 0.09 (Figure 7). There was a statistical difference at T2 for the group of patients with complete cleft and for the group formed by the entire pool of patients. The value of P = 0.067 was obtained for the comparison between the control group and the group of patients with incomplete cleft.
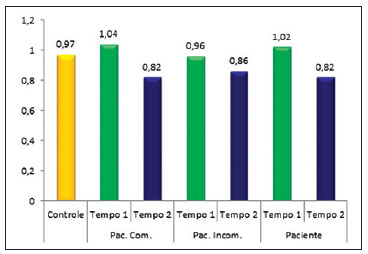
Figure 7 - Plot comparing height at ¼ of the medial nose width between the control group and patients with complete cleft (Pat. Comp.), with incomplete cleft (Pat. Incomp.), and all patients pooled into a single group (Patient).
With regard to the height of the base of the nose, the patients had a value of 0.89 ± 0.31 at T1 and 0.91 ± 0.36 at T2. Individually, the patients with complete cleft had a relationship of 0.92 ± 0.32 at T1 and 0.88 ± 0.35 at T2. The patients with complete cleft had values of 0.79 ± 0.26 at T1 and 0.99 ± 0.43 at T2. In the control group, the relationship was 0.96 ± 0.15. There was no statistical difference between the height of the base of the nose between the control group and any of the other groups (Figure 8).
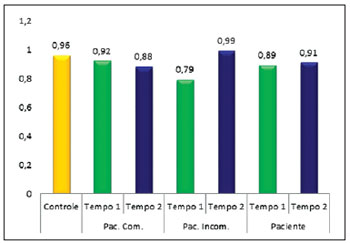
Figure 8 - Plot comparing height of the base of the nose between the control group and patients with complete cleft (Pat. Comp.), with incomplete cleft (Pat. Incomp.), and all patients pooled into a single group (Patient).
Figures 9 to 12 illustrate some patients included in this series of cases.

Figure 9 - Immediate postoperative appearance after primary cleft lip repair using the Mohler technique.

Figure 10 - Late postoperative appearance (after 1 year) of primary cleft lip repair using the Mohler technique.
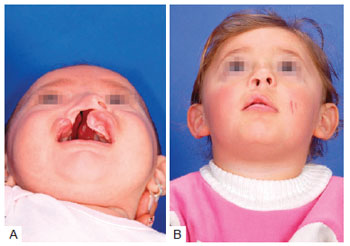
Figure 11 - In A, Preoperative appearance of a patient with complete right cleft lip and palate. A large alveolar gap of 13 mm is noticeable. In B, Postoperative appearance of the same patient at T2.
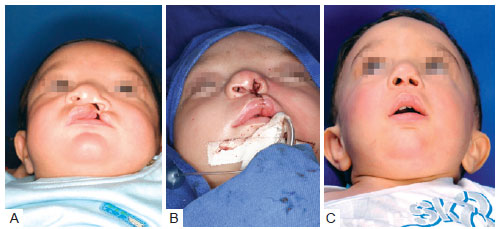
Figure 12 - In A, Preoperative appearance of a patient with complete left cleft lip and palate. In B, Postoperative appearance of the same patient at T1. Overcorrection of the nasal structures (nose height, height at ¼ of the medial width, height of the base of the nose) is noticeable. Restriction of the nose width and mimetization of the nose area were observed when compared to the nasal structures of the contralateral side. Overcorrection of nasal structures is important so as to obtain symmetry in the late postoperative period (at T2). In C, Postoperative appearance of the same patient at T2. The tendency of the nasal structures to relapse is noticeable.
DISCUSSION
Methods for quantifying results obtained after primary cleft lip repair surgery have been presented by numerous authors over the past 2 decades, and vary from visual inspection of the results in pairs to quantification of anatomical measures using 2-dimensional and, more recently, 3-dimensional photos. The quantification of surgical results done in pairs is a very subjective method, even though it is performed, in most cases, with predefined criteria14.
The quantification of results from photography in 2 dimensions and, more recently, in 3 dimensions is an objective method of analyzing results, although suitable equipment is necessary, as well as techniques for photographic patternization. Minimal changes in the distance between the photograph and the patient may lead to changes in the final measurements calculated in each photo. Therefore, obtaining mathematical ratios, as described by Wong et al.11, reduces the error that results from any change in the distance between photographer and patient. From the methods of quantifying results that have been suggested in the literature, quantification of measurements through 2-dimensional photography was chosen, because it is an objective, reliable, and reproducible method without the high financial costs of 3-dimensional photography.
Nasal deformity in cleft patients is caused by three important anatomical changes: nasal septum deviation, significant distortion of the alar cartilages caused by separation of the bone structures and soft tissues, and unleveling of the maxillary and alveolar bone resulting from the spreading of the palatal shelves. Unleveling of the bone of the alveolar arcades and maxilla exerts a vector of caudal force over a nasal wing, as well as over all nose structures; this is the greatest anatomical limitation to obtaining final nasal symmetry.
Cutting and Dayan7 described the inclusion of percutaneous sutures that exert a vector of force contrary to the primary caudal force originating from the alveolar gap resulting from the spreading of the palatal shelves. Nonetheless, the vector of caudal force may be higher than the vector generated by the percutaneous sutures. This phenomenon occurs mainly in serious cases that did not receive orthopedic correction of the maxilla. Relapse of the nasal deformity always occurs in these specific patients (serious cases without maxillary orthopedics).
Mulliken and Martínez-Pérez12 observed 23% postoperative nasal asymmetry in unilateral cleft patients. After modifying their technique to include the placement of an absorbable splint over the alar cartilage, they described a decrease in nasal asymmetry to 8.6%.
Numerous authors have described tactical modifications to obtain nasal symmetry in patients with unilateral cleft, but few have objectively quantified the efficacy of such modifications15-20. According to Kane et al.21, secondary nose surgery was needed in 30% to 40% of cleft patients; these evaluations were subjective and based on personal criteria. For that reason, Mulliken's parameters were used in this study to measure the anatomical structures and quantify the results. The nasal asymmetry index observed in this work (9.6%) was similar to the index observed by Mulliken and Martínez-Pérez12 (8.6%), who used an absorbable splint over the alar cartilage.
At the institution where this study was carried out, the cleft lip and palate patients are, for the most part, treated by the Sistema Único de Saúde (SUS); further, the absorbable splints are costly, making the procedure not financially feasible.
Data obtained in this study were compared to those obtained by Chang et al.13, who divided their cleft patients into four groups, each of which was submitted to a different therapeutic approach. Group I patients were treated by rhinoplasty without nasoalveolar molding (NAM); group II, NAM without intervention to the nose; group III, NAM with primary rhinoplasty; and group IV, NAM with extended primary rhinoplasty13.
Regarding nose height, we observed that the general group formed by all our patients had a relationship of 0.83, resembling group II from Chang et al.13 Similar results were obtained even when we stratified the groups into complete and incomplete cleft.
For nose width, the result was 1.21, which is statistically indistinguishable from the results of group I from Chang et al.13.
Individually, with regard to nose width, the patients with incomplete cleft had an index of 1.07. The patients with complete cleft had an index of 1.24, showing a tendency toward enlargement of the base of the nose in patients with a complete cleft. This phenomenon is most likely a consequence of the difference in bone structure in patients with a complete cleft.
Concerning the results of the ratio between the height at ¼ of the medial width and the nose width, the index was 0.82, similar to the data obtained for group II by Chang et al.13 Individually, the results were 0.85 for the patients with incomplete cleft and 0.81 for patients with complete cleft.
As to the height of the base of the nose, an index of 0.9 was observed, higher than the results presented by Chang et al.13, for all groups.
We also observed that, with regard to the nose area, the index of all the patients was 9.62% in T2, which was similar to that of the control group (7.24%). Additionally, it was observed that even without a statistical difference between the nose area in T1, the difference tended to approach the values obtained in the control group.
Concerning the nose height, it was observed that even when overcorrecting this parameter, with time there was a global reduction of height with a gradual increase in nose width, which can be explained by the anatomical changes inherent in the cleft patient and by the fact that the patients had not received maxillary orthopedics or even used a nasal tutor adapted to overcorrection.
Where the height of the base of the nose is concerned, there were no statistical differences, which shows that the treatment of the upper lip through the Mohler technique is enough to ensure symmetry at the base of the nose.
CONCLUSIONS
Obtaining primary nasal symmetry in patients subjected to cleft lip repair is a great challenge for the plastic surgeon and should be pursued obsessively by those seeking excellence in their results. The present study demonstrated that even when the principles proposed by Millard, Mohler, and Mulliken, among others, are respected, there was a tendency for relapse in the nasal region, mainly in patients with complete cleft. Therefore, new techniques should be researched to add to those already known, aiming at obtaining more harmonious results where nasal symmetry is concerned.
The search for excellent results associated with low surgical costs and different methods for analysis of results, comparing late postoperative results with control groups, may reveal details until now unnoticed by pioneer researchers on the topic and motivate young surgeons and researchers who are dedicated to the difficult, yet rewarding, task of dealing with the challenges of cleft lip and palate on a daily basis.
ACKNOWLEDGMENTS
To the members of the contest prize selection committee of the Brazilian Society of Plastic Surgery (SBCP) and to the reviewers of the Brazilian Magazine of Plastic Surgery, for the critiques and editorial suggestions. To resident Frederico F. Marques, for creating the artistic illustrations in this article.
REFERENCES
1. Boo-Chai K. An ancient Chinese text on a cleft lip. Plast Reconstr Surg. 1966;38(2):89-91.
2. Lemos PC. Nova operação para lábio leporino simples. O Hospital. 1956;1(4):607-11.
3. Spina V, Lodovici O. Conservative technique for treatment of unilateral cleft lip: reconstruction of the midline tubercle of the vermilion. Br J Plast Surg. 1960;13:100-7.
4. Spina V, Psillakis JM, Lapa F, Ferreira MC. Classificação das fissuras lábio palatinas: sugestão de modificação. Rev Hosp Clin Fac Med S Paulo. 1972;27(1):5-6.
5. Millard Jr DR. Saving faces. Autobiography. Boston: Write Stuff Enterprises; 2003.
6. Mohler LR. Unilateral cleft lip repair. Plast Reconstr Surg. 1987;80(4): 511-7.
7. Cutting CB, Dayan JH. Lip height and lip width after extended Mohler unilateral cleft lip repair. Plast Reconstr Surg. 2003;111(1):17-23.
8. Millard Jr DR. Complete unilateral clefts of the lip. Plast Reconstr Surg Transplant Bull. 1960;25:595-605.
9. McComb H. Treatment of the unilateral cleft lip nose. Plast Reconstr Surg. 1975;55(5):596-601.
10. Cutting C. Cleft lip nasal reconstruction. In: Rees T, LaTrenta G, eds. Aesthetic plastic surgery. Philadelphia: Saunders; 1994. p.497-532.
11. Wong GB, Burvin R, Mulliken JB. Resorbable internal splint: an adjunct to primary correction of unilateral cleft lip-nasal deformity. Plast Reconstr Surg. 2002;110(2):385-91.
12. Mulliken JB, Martínez-Pérez D. The principle of rotation advancement for repair of unilateral complete cleft lip and nasal deformity: technical variations and analysis of results. Plast Reconstr Surg. 1999;104(5):1247-60.
13. Chang CS, Por YC, Liou EJ, Chang CJ, Chen PK, Nordhoff MS. Long term comparison of four techniques for obtaining nasal symmetry in unilateral complete cleft lip patients: a single surgeon's experience. Plast Reconstr Surg. 2010;126(4):1276-84.
14. Noordhoff MS. Reconstruction of vermilion in unilateral and bilateral cleft lips. Plast Reconstr Surg. 1984;73(1):52-61.
15. Bearn DR, Sandy JR, Shaw WC. Photogrammetric assessment of the soft tissue profile in unilateral cleft lip and palate. Cleft Palate Craniofac J. 2002;39(6):597-603.
16. Raposo-do-Amaral CE. Avaliação do percentual de assimetria labial e nasal em pacientes com fissura labiopalatina submetidos à queiloplastia primária. Rev Bras Cir Plást. 2010;25(1):38-48.
17. McComb HK, Coghlan BA. Primary repair of the unilateral cleft lip nose: completion of a longitudinal study. Cleft Palate Craniofac J. 1996,33(1):23-30.
18. Salyer KE. Primary correction of the unilateral cleft lip nose: a 15-year experience. Plast Reconstr Surg. 1986;77(4):558-68.
19. Salyer KE. Early and late treatment of unilateral cleft nasal deformity. Cleft Palate Craniofac J. 1992;29(6):556-69.
20. McComb H. Primary correction of unilateral cleft lip nasal deformity: a 10-year review. Plast Reconstr Surg. 1985;75(6):791-9.
21. Kane AA, Pilgram TK, Moshiri M, Marsh JL. Long-term outcome of cleft lip nasal reconstruction in childhood. Plast Reconstr Surg. 2000;105(5):1600-8.
1. Aspiring member in training of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society for Plastic Surgery) - SBCP, resident physician in plastic surgery from the Prof. Dr. Cassio M. Raposo do Amaral Plastic Surgery Service of the Hospital SOBRAPAR - Crânio e Face (SOBRAPAR Craniofacial Surgery Institute), Campinas, SP, Brazil.
2. Associate member of SBCP, preceptor of the residents of the Prof. Dr. Cassio M. Raposo do Amaral Plastic Surgery Service of the Hospital SOBRAPAR - Crânio e Face (SOBRAPAR Craniofacial Surgery Institute), Campinas, SP, Brazil.
3. Named member of SBCP and of the Associação Brasileira de Cirurgia Crânio-Maxilo-Facial (Brazilian Association of Craniofacial Surgery) - ABCCMF, Master of Surgery from Universidade Estadual de Campinas (State University of Campinas), manager of the Prof. Dr. Cassio M. Raposo do Amaral Plastic Surgery Service of the Hospital SOBRAPAR - Crânio e Face (SOBRAPAR Craniofacial Surgery Institute), Campinas, SP, Brazil.
4. Plastic surgeon, Vice-President of the Hospital SOBRAPAR - Crânio e Face (SOBRAPAR Craniofacial Surgery Institute), named member of SBCP and ABCCMF, supervisor of the craniofacial surgery department of SBCP, Campinas, SP, Brazil.
Cassio Eduardo Raposo-do-Amaral
Hospital de Crânio e Face SOBRAPAR
Av. Adopho Lutz, 100 - Cidade Universitária
Campinas, SP, Brazil - CEP 13083-880 - CP 6028
E-mail: cassioraposo@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 27, 2011
Article accepted: March 13, 2012
Study conducted at the Prof. Dr. Cassio M. Raposo do Amaral Plastic Surgery Service of the Hospital SOBRAPAR - Crânio e Face (SOBRAPAR Craniofacial Surgery Institute), Campinas, SP, Brazil.
Study presented at the 48th Brazilian Plastic Surgery Congress, taking place at Goiânia, GO, Brasil, from 11 to 15 November 2011.
Winning study of the Silvio Zanini prize 2011.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter