INTRODUCTION
Reconstruction of the nipple-areola complex (NAC) is an essential step during breast
reconstruction. It usually occurs three to four months after the procedure that
restores the volume and contour of the breast.1 This surgery is indicated in cases where this complex is
amputated during mastectomies in order to ensure a more natural appearance to
the
reconstructed breast.
The first report was made in 1946 by Berson, and three triangular skin flaps were
used to perform this procedure. Soon after, there was the publication by Adams
in
1949, which also addressed new techniques for NAC reconstruction. In 2005, an
update
on NAC reconstruction was published by Farhadi et al., who pointed out four basic
principles for achieving success in this surgery, namely:
1 - The time for breast reconstruction would be approximately 3 to 4 months after
breast reconstruction2;
2 - In a unilateral reconstruction, the collateral nipple should serve as a model,
adapting only the position and asymmetries of the residual breast;
3 - In a bilateral reconstruction, the location is based on the relative and
preferred anatomical landmarks of each patient;
4 - The loss of nipple projection due to contraction of the structure during the
healing period must be anticipated, and there may be a correction that exceeds
the
desired result with local flaps by 25 to 50%.
In the literature, between the months of February and August 2020, approximately 92
articles were described that described new NAC3 techniques. There are more than 60 different technique
counts that have been described in the last 8 decades.
Since then, numerous techniques have emerged with the aim of improving contralateral
symmetry in position, size, shape, texture, and pigmentation. Today, NAC
reconstruction is a greatly enhanced procedure with techniques such as star flap,
skate flap, arrow flap, S-flap, CV flap, cylindrical flap, and double opposing
flap,
among others3.
Furthermore, it is necessary to mention the contraindications and complications of
this procedure, such as performing NAC before the completion of breast
reconstruction, especially when the final shape and volume have yet to be defined.
The main complication is the loss of nipple projection through local flaps since
it
is close to or in previous scars, and the blood supply may be damaged, with 45%
to
75% of the projection being predicted, making it an unpredictable complication.
In
addition, appearance and asymmetry are existing risks that should always be
discussed preoperatively4.
Therefore, it was necessary to create synthetic models to improve the technique, such
as the “training model in zone IV of the TRAM flap”, published in the
Revista Brasileira de Cirurgia Plástica, which was tested with
residents between 2006 and 2009 and showed that the skills acquired during training
with the model were transferred to the operating rooms4.
With this same purpose, the low-cost synthetic model for NAC training and simulation
was created to reduce the learning curves of the techniques, making it simpler
for
professionals in operating room situations. This model covers techniques such
as CV
Flap, Star Flap, and Skate Flap, among others, and is easily reused, which generates
an exponential growth curve since training in this model becomes unlimited4,5.
OBJECTIVE
This article aims to present a synthetic, novel and practical model for training in
reconstruction techniques of the nipple-areola complex, developed to be easy to
perform and low cost.
METHOD
To build the model, we needed a female bust mannequin, 1 and 2 cm thick foam sheet,
mesh fabric (96% polyester, 4% elastane), scissors, hot glue, Styrofoam glue,
and
sewing material.
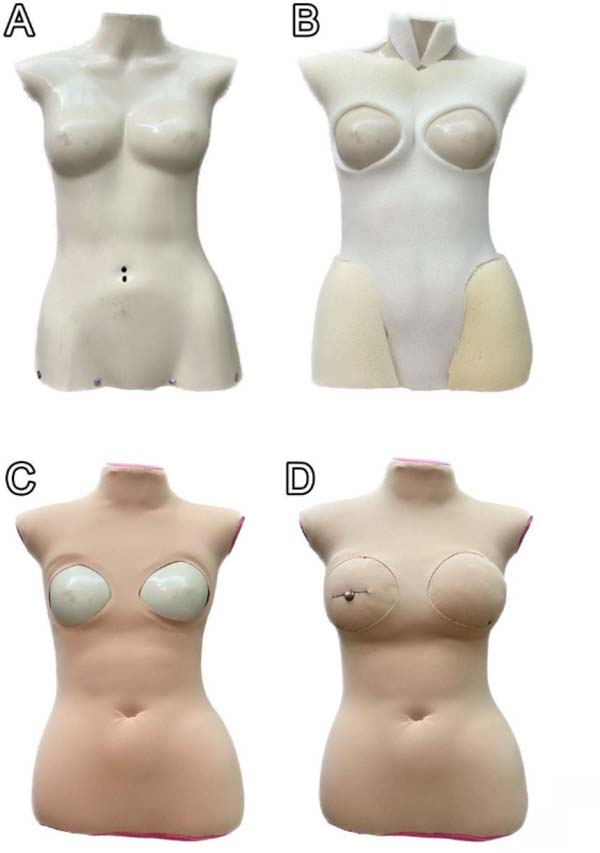
Initially, the assembly consisted of lining the mannequin using foams of different
thicknesses and hot glue and then covering it with the mesh fabric to finish it
off
(Figures 1A and 1B), leaving 2 circular openings in the breast region for later
positioning of the model’s refill parts (Figures 1C and 1D).
Figure 1 - Model construction stages. A. Complete mannequin; B. Covering the
mannequin with mesh fabric; C. Space marked for practicing the synthetic
model; D. Complete positioning of the breasts for practicing and
recharging the model.
Figure 1 - Model construction stages. A. Complete mannequin; B. Covering the
mannequin with mesh fabric; C. Space marked for practicing the synthetic
model; D. Complete positioning of the breasts for practicing and
recharging the model.
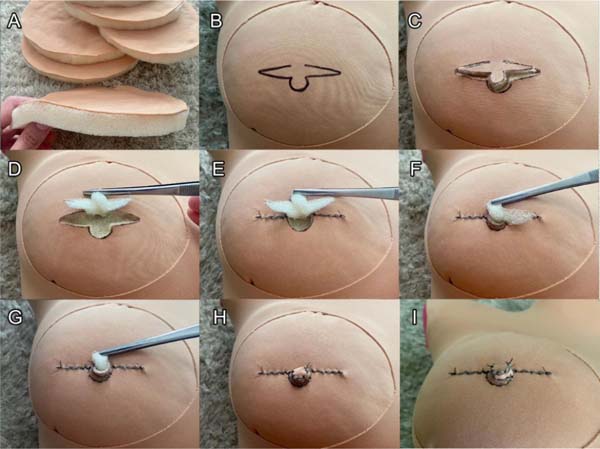
The refill pieces were made by gluing a circular piece of mesh to the 2 cm thick foam
sheet with the aid of Styrofoam glue (Figure 2A) so as to allow the simulation of the skin and subcutaneous tissue.
Figure 2 - Demonstration of the practice of reconstruction of the nipple-areola
complex (NAC) using the proposed model via the CV Flap technique. A.
Simulation of the skin and subcutaneous tissue; B. Demarcation of the
NAC flap to perform the CV Flap technique; C. Incision at the previously
marked site; D. Detachment of the skin and subcutaneous tissue while
maintaining the pedicle; E. Suturing of the NAC edges; F. First
approximation of the lateral “wings” of the flap; G. Second
approximation of the lateral “wings” of the flap; H. Central closure
with creation of the papilla protrusion; I. Suturing of the flap and
secondary defect.
Figure 2 - Demonstration of the practice of reconstruction of the nipple-areola
complex (NAC) using the proposed model via the CV Flap technique. A.
Simulation of the skin and subcutaneous tissue; B. Demarcation of the
NAC flap to perform the CV Flap technique; C. Incision at the previously
marked site; D. Detachment of the skin and subcutaneous tissue while
maintaining the pedicle; E. Suturing of the NAC edges; F. First
approximation of the lateral “wings” of the flap; G. Second
approximation of the lateral “wings” of the flap; H. Central closure
with creation of the papilla protrusion; I. Suturing of the flap and
secondary defect.
After completion, the flap is marked in the nipple-areola region with a fine-tipped
brush (Figure 2B), making it possible to
practice the various techniques described in the literature.
The model creation process was carried out by the plastic surgery academic league
of
the University of Fortaleza (UNIFOR) at the beginning of the 2023 academic semester,
with an average cost of R$175.50, with a recharge cost of approximately R$83.07
per
training session. The process between the development of the idea and the completion
of the model took around 30 days.
The model was presented to the plastic surgeon who teaches and advises the UNIFOR
Plastic Surgery Academic League and was approved and recommended for low-cost
simulation of the procedure. Furthermore, it is worth noting that the study did
not
involve humans or animals, so, in accordance with the Helsinki principles, there
was
no need for permission from the Research Ethics Committee to build the model,
which
was obtained using synthetic and disposable materials.
RESULTS
Academics demonstrated interest in carrying out the procedure after an
extracurricular theoretical class on techniques for reconstructing the nipple-areola
complex.
The experiment developed a model for simulating a specific technique for
reconstructing the nipple-areola complex without restrictions on the use of the
synthetic model and material.
Regarding the shape of the areola and the materials used to resemble the structure
of
the local cutaneous and subcutaneous tissue, it was observed that the synthetic
model was easy to handle in practice and, consequently, it was completely simulated
due to the structure used, enabling training in the CV Flap technique, which
requires incision, detachment, maintaining the pedicle and suturing of the
flaps.
DISCUSSION
Surgical knowledge in undergraduate medical courses is a relevant issue, especially
in relation to its practical application, due to the lack of economically accessible
methods that can simulate the process in question, in addition to the limited
time
spent on learning such procedures. In this context, simulation in the practical
setting offers several benefits for learning at different levels of knowledge,
providing better performance in the surgical environment due to the skills covered
by the training models.
It is known that a surgical curriculum presupposes repetitive training of such
techniques, with the aim of developing the necessary fine manual skills, especially
in students whose contact with the surgical center is restricted, such as the
skills
exemplified in stages B to I in Figure 2. Thus,
in a complementary way to the traditional learning model based on long internships
and dependent on the master-apprentice relationship, the alternative method
presented in the present study proposes the construction of an anatomical breast
simulator that makes it possible to mirror the real surgical scenario, allowing
the
repeated execution of the reconstruction of the nipple-areola complex, with an
acceptable level of fidelity6.
According to Santos et al.7, the
benefits of simulation experience for residents or undergraduate students are
varied. The low cost of production and maintenance of the model democratizes access
to this type of training beyond the high-cost synthetic models, exposing the student
to situations similar to the real context, thus reducing iatrogenic and aesthetic
complications for patients, in addition to ethical issues7.
Among the brief limitations of the proposed prototype, the inconvenience that may
restrict its widespread use is the need for a certain amount of sewing expertise
for
its construction, although reusing a mannequin saves a great deal of time spent
on
manufacturing, as can be seen in finishing stages B and C in Figure 1.
In comparison to training models that use fresh cadavers and animal parts, the
creation of a synthetic model replaces the ethical impasse in the effort to search
for inputs that have maximum similarity to human tissue, such as the simulator
by
Jefferson et al.8, which equates
the use of synthetic skin to pig skin as handling objects for training.
The arrangement of materials in the proposed synthetic model simulates the structure
of the cutaneous and subcutaneous tissue, enabling the practice of techniques
effectively described in the literature and providing easy handling of the flap
and
the incision with a scalpel. Furthermore, the use of easily replaceable materials
differs positively from the organic models proposed by scholars who use, for
training plastic surgery residents, flaps from post-mortem animals, such as chicken
skin, beef tongue, discarded porcine tissues, and even symbiotic yeast cultures,
making the experience limited to use due to the lack of availability of the
material9.
Regarding the financial investment related to its architecture, as well as the
reinstallation of synthetic breasts for new sutures, mentioned in steps C and
D of
Figure 1, the selected materials allow for
almost unlimited reuse of the simulator by academics and supervising surgeons
due to
the low cost of the main inputs, such as mesh, Styrofoam glue, and sponge sheet.
Comparatively, anatomical models of great contemporary relevance, such as those
that
use three-dimensional (3D) printing, require additional costs in technology that
are
inaccessible to a large portion of the academic population. The approval by renowned
plastic surgeons of the new simulator created successfully, demonstrated the quality
of this low-cost synthetic model, despite its simplicity10.
CONCLUSION
The proposed synthetic model for the reconstruction of the nipple-areola complex has
great potential to aid in the training and improvement of available surgical
techniques for the procedure since it can accurately simulate the steps of the
real
surgical procedure. In addition, it has proven to be a tool that provides gains
in
terms of accessibility and low manufacturing costs.
REFERENCES
1. Lamartine JD, Cintra Junior R, Daher JC, Cammarota MC, Galdino J,
Pedroso DB, et al. Reconstrução do complexo areolopapilar com double opposing
flap. Rev Bras Cir Plást. 2013;28(2):233-40.
2. Balbinot P, Ono MCC, Groth AK, Silva ABmD. Reconstrução do complexo
areolopapilar e da mama com colocação de implante no mesmo tempo cirúrgico. Rev
Bras Cir Plást. 2013;28(3 Suppl.1):65.
3. Paolini G, Firmani G, Briganti F, Sorotos M, Santanelli di Pompeo F.
Guiding Nipple-Areola Complex Reconstruction: Literature Review and Proposal
of
a New Decision-Making Algorithm. Aesthetic Plast Surg.
2021;45(3):933-45.
4. Gomes AAR, Pessoa BBGP, Pessoa SGP. Nipple-areola complex
reconstruction: training bench model in zone IV TRAM flaps. Rev Bras Cir Plást.
2010;25(2):379-80.
5. Strassburger CP, Ramos RFMR. Nipple-areola complex reconstruction:
What we have today? Rev Bras Mastologia. 2016;26(1):18-23.
6. Pacífico AACP, Correia AS, Borges BMC, Costa MB, Arrais MPFF,
Carneiro SL, et al. Low-cost synthetic model for skin flap training. Rev Bras
Cir Plást. 2020;35(3):304-8.
7. Santos NEB, Lima, EB, Sales MA, Vieira APSB, Melo RB, Sá CDL. A
utilização de modelos de simulação para treinamento cirúrgico - revisão
integrativa. Res Soc Dev. 2021;10(2):e21210212420.
8. Jefferson IS, Robinson SK, Surprenant D, Whittington A, Arshanapalli
A, Tung-Hahn E, et al. Surgical training tools for dermatology trainees: porcine
vs. synthetic skin for excision and repair. Arch Dermatol Res.
2021;313(9):793-7.
9. Dreven VA, Garner SJ, MacDermott ST, Yates MW, Costa SG, et al. Will
SCOBY do? An alternative for teaching basic surgical skills of suturing and skin
excision. J Surg Simul. 2018;5(99):99-104.
10. Garcia TR, Macedo RM, Vaz MHV, Borges GHI, Zendron IM, Arruda JT.
Impressão 3D de peças anatômicas como ferramentas de educação e auxílio na
prática clínica. Res Soc Dev. 2022;11(13):e248111335234.
1. Universidade de Fortaleza, Medicina, Fortaleza,
CE, Brazil
Pedro Lucena de Aquino Av.
Washington Soares, 1321, Edson Queiroz, Fortaleza, CE, Brazil., Zip Code:
60911-905, E-mail: pedrolucena@edu.unifor.br
Artigo submetido: 08/02/2023.
Artigo aceito: 26/07/2024.
Conflicts of interest: none.