

Original Article - Year 2024 - Volume 39 -
Breast reconstruction: 10 years experience
Reconstrução mamária: Experiência de 10 anos
ABSTRACT
Introduction: Breast reconstruction after surgical treatment for breast cancer (one of the main cancers that affect women) has been progressively more recommended, given the benefits of psychological recovery and quality of life, whether using implants and/or autologous tissues. The present work aims to demonstrate the team's experience, and discuss operative techniques and complications concerning data from the world literature, in addition to verifying the applicability of the technique in the team's clinical practice.
Method: Retrospective observational study developed at a university hospital in Juiz de Fora based on a review of medical records of patients who underwent mastectomy with breast reconstruction between 2010 and 2020.
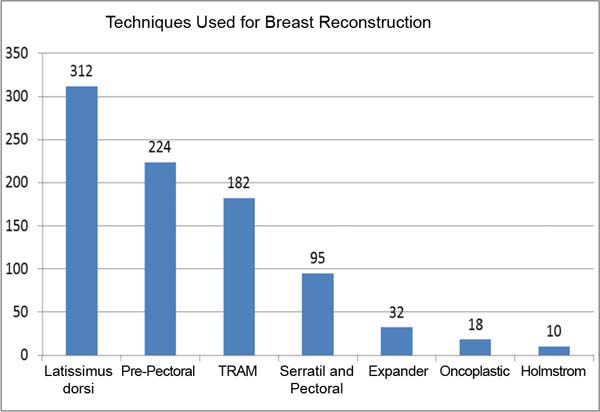
Results: Of the 860 breasts treated, 84% underwent immediate oncological surgery and 16% were late; the main access to the breast tissue was the Stewart incision, followed by extended inframammary, periareolar, and inverted T incisions; regarding reconstructive techniques, 35% of cases used a latissimus dorsi muscle flap, 25% used a prepectoral prosthesis, 20% used a transverse rectus abdominis myocutaneous flap and 10% used a local muscle flap. The most common complications were surgical site dehiscence, followed by skin necrosis, seroma, surgical site infection, and hematoma, in addition to other less common complications such as chronic pain and prosthesis rupture after mammography.
Conclusion: Postmastectomy breast reconstruction is essential for a woman's physical and emotional recovery, with the techniques used in the last ten years being consistent, reliable, with low morbidity, and with excellent aesthetic results when correctly indicated.
Keywords: Breast; Mammaplasty; Breast neoplasms; Surgical flaps; Muscles; Postoperative complications; Plastic surgery procedures.
RESUMO
Introdução: A reconstrução mamária pós-tratamento cirúrgico do câncer de mama (um dos principais cânceres que acometem as mulheres) tem sido progressivamente mais indicada, haja vista o benefício da recuperação psicológica e da qualidade de vida, seja utilizando implantes e/ou tecidos autólogos. O presente trabalho visa demonstrar a experiência da equipe, discutir técnicas operatórias e complicações em relação aos dados da literatura mundial, além de verificar a aplicabilidade da técnica na prática clínica da equipe.
Método: Estudo observacional retrospectivo desenvolvido em hospital universitário em Juiz de Fora a partir da revisão de prontuários de pacientes submetidas a mastectomia com reconstrução mamária entre 2010 e 2020.
Resultados: Das 860 mamas abordadas, 84% foram imediatas à cirurgia oncológica e 16% foram tardias; o principal acesso ao tecido mamário foi a incisão de Stewart, seguido de incisões inframamárias estendidas, periareolares e T invertido; quanto às técnicas reconstrutoras, destaca-se 35% dos casos com retalho com músculo grande dorsal, 25% com prótese pré-peitoral, 20% com retalho miocutâneo transverso do músculo reto abdominal e 10% com retalho muscular local. As complicações mais incidentes foram deiscência de sítio cirúrgico, seguida de necrose cutânea, seroma, infecção de sítio cirúrgico e hematoma, além de outros menos comuns como dor crônica e ruptura de prótese após mamografia.
Conclusão: A reconstrução mamária pós-mastectomia é indispensável para a recuperação física e emocional da mulher, sendo as técnicas utilizadas nos últimos dez anos consistentes, confiáveis, de baixa morbidade e com ótimos resultados estéticos quando bem indicadas.
Palavras-chave: Mama; Mamoplastia; Neoplasias da mama; Retalhos cirúrgicos; Músculos; Complicações pós-operatórias; Procedimentos de cirurgia plástica.
INTRODUCTION
Breast cancer, except non-melanoma skin tumors, is the main cause of neoplasia in women in Brazil, in much of the world, and also the one with the highest lethality. Therefore, it is a public health problem1.
Estimates reveal that, in the 2020-2022 biennium, there would be an incidence of 66,280 new cases, corresponding to 29.7% of cancers in women, with survival and prognosis closely related to access to the health system, early diagnosis, and adequate treatment1.
Treatment is based on local therapies (surgery and radiotherapy) and systemic therapies (chemotherapy, hormone therapy, and biological therapy)2. The application of immediate breast reconstruction is increasingly recommended, given the advancement of adenomastectomy, sparing the total or partial skin envelope (nipple-sparing or skin-sparing, respectively), which guarantees better quality and quantity of skin for reconstructions. with prostheses or even with autologous tissue, at the same surgical time. Therefore, currently, the restoration of the shape, contour, and volume of the breast concomitantly with mastectomy is a reality, as well as a key point in the psychological recovery and quality of life, even if partial, in the face of the disease3,4.
The most commonly used procedures in breast reconstruction use implants and/or autologous tissue. These are the pedicled myocutaneous flap of the latissimus dorsi (LD), transverse myocutaneous flap of the rectus abdominis muscle (TRAM), local muscular flap (LF), and the use of alloplastic materials (expanders and silicone prostheses). Although we know the benefits of their applicability in immediate breast reconstruction, these techniques are not free from complications such as seromas, hematomas, surgical wound infection, flap necrosis, prosthesis extrusion, and capsular contracture. And, sometimes, they are related to comorbidities such as smoking, surgical technique in adenomastectomy (especially care regarding the thickness and regularity of the skin flap), the expertise of the team involved in breast reconstruction, and the application of radiotherapy and chemotherapy5,6.
OBJECTIVE
The present work aims to demonstrate the team’s experience in post-mastectomy breast reconstruction with prosthesis or with autologous tissue with or without a breast implant, discuss operative techniques and complications concerning data from the world literature to, finally, verify the applicability of the technique in the team’s clinical practice.
METHOD
We analyzed, through a retrospective review of medical records, 791 female patients who underwent mastectomy with immediate or delayed breast reconstruction from January 2010 to June 2020. The project was approved by the Research Ethics Committee (opinion number 5,660,021 ). The techniques of TRAM, LD, LF (serratus anterior and pectoralis major), expander, reverse expander, oncoplastic, lateral thoracic fasciocutaneous flap (Hölmstrom), and reconstruction with prepectoral implant were used, techniques associated or not with silicone implants. When used, breast implants were natural or round in shape, had high or extra-high projection, and had a textured surface.
The reconstruction technique applied was decided together with the patients and by analyzing some factors. Patients undergoing modified radical mastectomy with a donor abdomen, non-smokers, and without impeding abdominal scars were candidates for reconstruction with TRAM. Patients without these conditions and intending to become pregnant were selected for reconstruction with LD. And those who requested minor surgery or with important comorbidities such as lung disease and heart disease were indicated for LF or Hölmstrom flap.
In cases of patients undergoing skin-sparing or nipple-sparing mastectomy, with total or partial preservation of the skin envelope, reconstruction with a prepectoral prosthesis was chosen, as long as the skin flap was of sufficient thickness. When the flap was excessively thin, it was decided to use the implant in conjunction with an LF or partially filled skin expander during surgery. Furthermore, some cases received a skin expander for salvage surgeries and late reconstructions, in patients who did not have a donor area or did not want another technique.
Factors such as age, laterality, comorbidities, smoking, mastectomy technique, types of incisions, the timing of reconstruction (immediate or delayed), complications (seroma, hematoma, infection, necrosis, dehiscence, and prosthesis exposure), and need for a second surgery were analyzed. (change of prosthesis size, reconstruction of the nipple-areolar complex - NAC, contralateral breast symmetrization, fat grafting, capsulotomy, or capsulectomy).
RESULTS
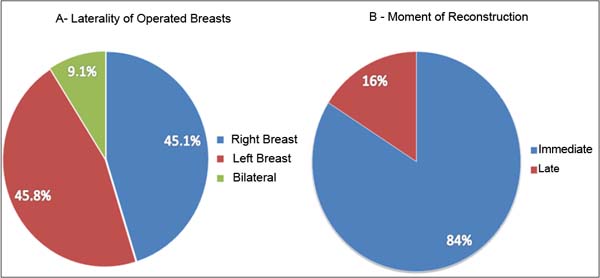
The number of patients operated on during the period was 791 cases, between 27 and 79 years old, with an average of 51 years old, with follow-up time varying between five months and ten years and 11 months, which corresponded to a total of 860 reconstructed breasts; 356 approaches to the right breast, 360 to the left breast and 72 bilateral cases (Figure 1), 84% immediate reconstructions and 16% late reconstructions (Figure 1).
Regarding the access route to the breast tissue, 498 Stewart-type incisions were used; 217 extended inframammary incisions; 75 periareolar; 37 inverted T, and 33 incisions in the upper external quadrant. 498 modified radical mastectomies were performed; 244 nipple-sparing; 95 skin-sparing; 15 prophylactic mastectomies and 8 quadrantectomies.
Regarding the breast reconstruction technique used, 35.7% were reconstructions with LD, 25.6% with prepectoral prosthesis, 20.8% with TRAM, 10.9% with LF (serratus anterior and pectoralis major), 3 .8% with expander; 2% oncoplastic; and 1.1% Hölmstrom flap (Figure 2).
The reconstruction techniques with prepectoral prosthesis, LD, LF, and Hölmstrom flap used a silicone prosthesis with a volume between 155 and 640ml (average of 351), 85% with a natural profile, and 15% round.
The main comorbidities found in patients were hypertension, diabetes, hypothyroidism, depression, and obesity. In 5% of patients (44 cases) smoking was active at the time of reconstruction.
When it comes to complications related to the use of implants, the most notable is the loss of the prosthesis in 70 patients (20 cases due to necrosis, 25 due to post-chemotherapy seroma infection, and 25 due to surgical wound dehiscence) and contracture grades II, III and Baker IV in 52 cases.
In TRAM reconstructions, there were six cases of abdominal bulging, two cases of abdominal hernia, and three cases of seroma in the donor area.
In general complications, 45 cases of surgical wound dehiscence were identified, 32 cases of skin necrosis due to mastectomy, 30 cases of seroma in the recipient area, and 12 cases in the donor area (three when TRAM and nine when LD), 27 cases of surgical site infection, eight cases of hematoma, two cases of partial flap necrosis with good evolution, four cases of total flap necrosis, two cases of large liponecrosis, one case of post-mammogram prosthesis rupture, three cases of pain chronic and one case of paraplegia due to extradural hematoma.
A second surgical procedure was necessary for 258 patients, distributed as follows: 17 prosthesis exchanges, 51 NAC reconstructions, 97 contralateral breast symmetrizations, 38 fat grafts, 27 capsulotomies or capsulectomies, 10 prosthesis repositionings, and 18 contralateral risk-reducing surgeries.
In the long term, 20 patients had tumor recurrences, 10 patients developed a second primary tumor in the contralateral breast, 16 patients had metastases, five patients underwent salvage reconstruction with an expander after loss of the prosthesis and three patients required placement of a new prosthesis.
DISCUSSION
Breast reconstruction is currently not restricted to the concept of breast cone reconstruction. The naturalness and similarity concerning the contralateral breast are highly valued by the team and the patient and, in this context, advances in techniques and alloplastic materials, when used, help with results3,7,8.
In the present study, the percentage of immediate reconstructions (84%) is in line with the current preference for applying immediate breast reconstruction to adenomastectomy, and the use of implants has grown in the same proportion. Studies show that 80% of reconstructions are immediate with prosthesis9,10. Although it is considered safe, effective, reliable, and can be used especially in women with various comorbidities, high rates of complications (capsular contracture and infection) with the use of prostheses are seen, especially if followed by radiotherapy9. In our 10-year series, the rate of prosthesis loss (8%) is in line with values found in the literature (7% - 9%), while the rates of seroma and capsular contractures are considerably lower (6% and 5% against 12 - 21% and 19% respectively)6.
Meta-analyses by Toh et al.11 and Gurrado et al.10 showed that there was no statistical significance between the rates of infection, seroma, hematoma, and capsular contracture between immediate reconstruction with prosthesis and two-stage expander-prosthesis reconstruction. However, the incidence of necrosis, reoperation, and loss of the prosthesis were higher in immediate reconstructions with prostheses.
In a ten-year retrospective analysis, Mak & Kwong5 collected data from 243 patients who underwent immediate autologous and prosthetic breast reconstructions with a follow-up of approximately two years. Patients undergoing autologous reconstruction had lower complication rates (24.4%) than those undergoing reconstruction with a prosthesis (50%). Among the most relevant complications, bulging and abdominal hernia stand out (9.1%). In the present study, surgical site dehiscence was the main complication of this type of reconstruction (5.2% of operated cases).
A great advantage of reconstruction with autologous tissue is that aesthetic damage to the breast is less after radiotherapy3,4. In cases where immediate breast reconstruction is indicated, despite the certainty of adjuvant radiotherapy, reconstruction options should be based on tissue characteristics and blood supply and reconstruction options with autologous tissue should have priority as they reflect superior vascularization, resistance to radiation, better sensory recovery and lower failure rates4,6,8. However, factors such as team expertise, improvement in the target of the irradiated breast, and thickness of the skin flap in mastectomy directly influence these results4,8.
CONCLUSION
Breast reconstruction with alloplastic material or autologous tissue with or without a breast implant is an indispensable tool for a woman’s physical and emotional recovery. And, with good team preparation, the techniques are consistent, reliable, low morbidity, and with excellent aesthetic results when well indicated.
REFERENCES
1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Estimativa 2020: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2019.
2. Brasil. Ministério da Saúde. Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). A situação do câncer de mama no Brasil: síntese de dados dos sistemas de informação. Rio de Janeiro: INCA; 2019.
3. Toyserkani NM, Jørgensen MG, Tabatabaeifar S, Damsgaard T, Sørensen JA. Autologous versus implant-based breast reconstruction: A systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg. 2020;73(2):278-85.
4. Citgez B, Yigit B, Bas S.Oncoplastic and Reconstructive Breast Surgery: A Comprehensive Review. Cureus. 2022;14(1):e21763.
5. Mak JC, Kwong A. Complications in Post-mastectomy Immediate Breast Reconstruction: A Ten-year Analysis of Outcomes. Clin Breast Cancer. 2020;20(5):402-7.
6. Friedrich M, Krämer S, Friedrich D, Kraft C, Maass N, Rogmans C. Difficulties of Breast Reconstruction - Problems That No One Likes to Face. Anticancer Res. 2021;41(11):5365-75.
7. Siqueira HFF, Teixeira J, Lessa Filho R, Brito EAC, Lima M, Moura AR, et al. Aesthetic assessment of breast reconstruction in the eyes of plastic surgeons versus nonplastic physicians. Rev Assoc Med Bras. 2022;68(1):13-8.
8. Choi M, Frey JD. Optimizing Aesthetic Outcomes in Breast Reconstruction After Nipple-Sparing Mastectomy. Aesthet Surg J. 2020;40(Suppl 2):S13-21.
9. Ho TB, Wood WC, Mspt PDS. Breast Reconstruction in the Setting of Postmastectomy Radiotherapy: Controversies and Disparities. Oncology (Williston Park). 2019;33(12):688845.
10. Gurrado A, Pasculli A, Toma A, Maruccia M, Elia R, Moschetta M, et al. Mastectomy with one-stage or two-stage reconstruction in breast cancer: analysis of early outcomes and patient’s satisfaction. Updates Surg. 2023;75(1):235-43.
11. Toh U, Takenaka M, Iwakuma N, Akagi Y. Clinical outcomes of patients after nipple-sparing mastectomy and reconstruction based on the expander/implant technique. Surg Today. 2021;51(6):862-71.
1. Hospital Universitário da Universidade Federal de Juiz de Fora, Juiz de Fora, MG, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, Juiz de Fora, MG, Brazil
Corresponding author: Larissa Silva Leitão Daroda Rua Catulo Breviglieri, s/nº, Bairro Santa Catarina, Juiz de Fora, MG, Brazil, Zip Code: 36036-110, E-mail: larissadaroda@gmail.com
Article received: July 3, 2023.
Article accepted: December 5, 2023.
Conflicts of interest: none.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter