INTRODUCTION
The breasts are of fundamental importance in the patient’s psychosexual well-being,
since the desire to improve aesthetic appearance is part of self-care, whether to
reverse sagging, increase volume, rejuvenate, correct asymmetry, or reconstruct the
breasts1. Thus, the implantation of breast prostheses is one of the most performed surgeries
in the world, according to data released by the International Society of Aesthetic
Plastic Surgery (ISAPS), representing around 15.8% of aesthetic surgical interventions
carried out in 2018, worldwide2.
In 1889, Gersuny described breast augmentation with paraffin injection into the breast
parenchyma. Over time, various materials have been used to reconstitute breast volume,
such as ivory prostheses, sponges of different compositions, dermal-fat grafts, liquid
silicone, or gel3.
The introduction of silicone breast implants began in 1963, in the United States of
America, through Cronin and Gerow, and since then the aforementioned surgical intervention
has been the subject of great discussion4,5. The initial conception aimed at aesthetic surgeries, but currently the field of
breast reconstruction uses implants on a large scale6. The first implants were manufactured with thick elastomer, in two halves, which
were glued together to form a single piece. Over time, several evolutionary steps
were overcome7,8.
Sperli described 7 evolutionary phases of breast implants that depend on the type
of wrap, with or without patch, coating, and inflatable prostheses9,10. For most types of implants and styles, there have been variations over the years,
with single-lumen gel-filled implants being more common in our country6.
Despite improvements in surgical techniques and the safety of current implants, patients
are still faced with potential complications, the most frequently encountered of which
are hematomas, seromas, infections, asymmetries, rippling, and especially capsular
contractures, which are still the most commonly seen complications. with a global
incidence of around 27%, associated with the use of smooth and textured implants from
the first generations of prostheses11-13.
Although mammography and ultrasound are the exams initially requested for investigation,
nuclear magnetic resonance (NMR) is the most useful imaging modality for characterizing
breast implants, due to its high spatial resolution and the provision of a contrast
image between the implant and surrounding soft tissues14. Another advantage is the absence of ionizing radiation. NMR has greater sensitivity
(72-94%) and specificity (85-100%) to detect implant ruptures, thanks to its sequences
that can suppress or emphasize the signal from the silicone3.
In the MRI protocol, high-resolution devices, the internal composition of the silicone
is better visualized with details in a sagittal T2 FSE (Fast spin echo) image, and
the high-quality T2 image with water suppression can be useful to differentiate the
silicone with intracapsular rupture from the peri-implant fluid15. Two-plane imaging is indicated to differentiate early intracapsular ruptures from
folds formed at the bottom and top of the implant. Furthermore, imaging in the anteroposterior
plane is not recommended due to artifacts caused by the heart and chest15.
Unusual complications may occur, such as intracapsular and extracapsular ruptures,
late hematomas, and contour deformities, with magnetic resonance imaging being the
gold standard image evaluation for diagnostic elucidation16.
Seromas are uncommon late complications, but can occur without a defined cause, the
treatment of which involves the removal or replacement of prostheses17. The appearance of a large seroma more than one year after implant placement is defined
as late. In prospective studies, it was estimated that breast implant-related anaplastic
large cell lymphoma (BIA-ALCL) is common in late seroma presentations18. In the event of a late seroma that is not easily explained by infection or trauma,
the disease should be considered suspected19.
The most common type of rupture is that of the implant shell (elastomer envelope)20, the leak of which does not extend beyond the fibrous capsule that commonly forms
around silicone implants, accounting for 80 to 90% of all intracapsular implant ruptures
5. Extracapsular rupture is defined as the extrusion of both the shell and the fibrous
capsule, with macroscopic silicone leakage21-23.
OBJECTIVE
To survey the changes found in MRI scans of patients with silicone implants, and identify
unusual findings and their frequencies in a large radiology service.
METHOD
A retrospective survey was carried out in the registry of a private radiology clinic
in Brasília-DF of exams carried out on patients with silicone implants between April
2015 and March 2023.
This is a series of cases in which patients with alterations were identified and the
so-called “unusual” alterations were selected, due to their low frequency or absence
of citation in the literature, after surgeries to include a silicone prosthesis. Patients
who underwent breast augmentation using implants for aesthetic purposes or breast
reconstruction were included in the study.
The reason for carrying out the exam was not the subject of the study. A survey of
nuclear magnetic resonance (NMR) reports and images was carried out and those that
showed unusual findings were selected for study. Furthermore, a literature review
was carried out on each of the cases described and listed below.
Finally, it should be noted that the present study followed the principles contained
in the Declaration of Helsinki, developed by the World Medical Association. Furthermore,
the work was submitted and approved by the Ethics and Research Committee, under number
75934023.7.0000.0257.
RESULTS
211 patients with breast implants underwent MRI and changes were found in 12, which
corresponds to 5.68% of the total. A classification into 3 groups was used:
Group 1, with a total of 5 patients: 5 patients (2.3%) presented a large amount of
pericapsular fluid, 3 of which were cases of pericapsular seroma, submitted to aspiration
punctures and CD30 and ALK1 measurement, considering the possibility of IABP -ACL,
with 1 positive patient. Others 3 patients (1.4%) had capsular granuloma and 1 patient
(0.4%) had late capsular seroma with hemorrhagic content.
Group 2, with a total of 3 patients: 2 patients (0.9%) had axillary lymph node disease;
1 patient (0.4%) had intra and extracapsular rupture; 1 patient (0.4%) had a nodule
close to the fibrous capsule of the implant; 1 patient (0.4%) ipsilateral axillary
lymph node disease of probable inflammatory/infectious origin and 1 patient (0.4%)
intra-nodal silicone.
Group 3, with a total of 4 patients: 1 patient (0.4%) with pectoral muscle edema,
2 patients with desmoid tumor, and 1 patient (0.4%) with herniation of the fibrous
capsule.
Case 1
B.A.L.I., female, 25 years old, states that 5 years ago she underwent surgery to place
a prosthesis for aesthetic purposes for breast augmentation. She underwent surgery
with the apposition of implants in the retroglandular plane. Radiological finding:
bilateral pericapsular fluid, in greater quantity on the right, associated with enhancement
of the fibrous capsule. Given the possibility of BIA-A.L.C.L., the investigation continued
with ultrasound-guided needle aspiration, yielding a positive result.
Case 2
D.G., female, 69 years old, reports that she underwent breast reconstruction surgery
after a bilateral mastectomy with silicone implants in the retromuscular plane. An
MRI examination was performed with the finding of a large pericapsular seroma on the
right, suspicious for BIA-ALCL, a capsular nodular image with heterogeneous enhancement,
but probably corresponding to an induced silicone capsular granuloma. Furthermore,
there was a morphological change in the right prosthesis compatible with capsular
contracture.
Case 3
R.C.M., female, 71 years old, 22 years ago she underwent aesthetic breast surgery
with a silicone implant in the retroglandular plane. A routine examination revealed
a large pericapsular seroma with hyperproteic/hemorrhagic content on the right. FNAB
was performed, considering the possibility of BIA-ALCL. After this MRI examination,
this patient underwent bilateral capsulectomy surgery, with clot removal on the right
and breast reconstruction 1 year ago.
Case 4
J.M., female, 62 years old, states that 6 years ago she underwent breast augmentation
surgery with implants placed in the retroglandular plane. MRI revealed a nodule next
to the fibrous capsule of the left implant of non-specific origin, which may correspond
to a granuloma.
Case 5
K.A., female, 55 years old, undergoing reconstruction surgery due to a right mastectomy.
An MRI performed revealed enhancement of the breast parenchyma and implant capsule
on the left, associated with non-specific ipsilateral axillary lymph node disease,
probably inflammatory/infectious.
Case 6
R.C.S., 66 years old, states that 11 years ago she underwent cosmetic surgery for
breast augmentation with a retroglandular silicone prosthesis. MRI showed that the
left implant showed signs of capsular contracture. Absence of signs suggestive of
intra and extracapsular rupture of the implants.
Case 7
A.S., 46 years old, female, underwent aesthetic silicone breast implant surgery in
the retroglandular position 10 years ago. Presents silicone in the right breast with
a moderate amount of pericapsular fluid, in addition to thickening and diffuse enhancement
of the fibrous capsule.
Case 8
C.A.M., 52 years old, female, underwent breast reconstruction surgery due to bilateral
adenomastectomy using double lumen breast expanders, with signs suggestive of intracapsular
rupture on the left. In addition, on imaging exams, left axillary lymph node enlargement
is presented, with a heterogeneous signal, which may correspond to intra-nodal silicone,
suggesting ipsilateral extracapsular rupture.
Case 9
E.R., 49 years old, female, underwent cosmetic surgery 2 years ago with a breast implant
in the retroglandular plane. Imaging examinations showed marked thickening and diffuse
pericapsular enhancement, associated with morphological changes, a large pericapsular
seroma, and edema of the underlying pectoral muscle, with pre-sternal extension to
the medial aspect of the fibrous capsule and contralateral pectoral muscle.
Case 10
C.M., 47 years old, female, underwent breast reconstruction surgery with prosthesis
in the submuscular plane. On magnetic resonance imaging of the breasts, a breast expander
on the right of the usual shape, without signs of rupture, with diffuse capsular enhancement.
In the inferolateral quadrant of the right breast, there is a herniation of the fibrous
capsule with heterogeneous contents.
Case 11
B.K.A., 30 years old, female, underwent mammoplasty with the inclusion of implants,
for aesthetic purposes. One year after surgery, a hardened area was noticed in the
left breast. Magnetic resonance imaging was performed, finding a heterogeneous nodulation
in close contact with the implant capsule, with a positive result for desmoid tumor.
Case 12
L.M.F., 54 years old, female, underwent aesthetic surgery with an implant in the retroglandular
plane. She reported nodulation in the left breast, which presented an irregular and
spiculated appearance on MRI, with a result compatible with a desmoid tumor.
DISCUSSION
Faced with several complications related to breast implants, magnetic resonance imaging
is the method of choice for evaluating the integrity of silicone implants, as it is
more accurate than mammography and ultrasound, chosen for monitoring and cancer screening6. With a sensitivity of up to 94% in detecting rupture and specificity between 85%
and 100%, sequences with and without silicone suppression are used, as well as combined
sequences to evaluate parenchyma and prosthesis24.
In the evaluation of lesions in the breast parenchyma, paramagnetic contrast can be
used, which has better accuracy in recent post-operative breasts, due to the architectural
distortion and edema of the operated breast24. This usual change is seen when capsular contracture occurs, after breast augmentation
with silicone. The thin fibrous capsule normally forms around the prosthesis and causes
discomfort and deformity in the breast architecture15.
There are several signs found on MRI that correspond to complications of silicone
implants, with findings compatible with extracapsular rupture (keyhole sign or noix
sign) being described in the literature6. Furthermore, on the sagittal-weighted image, the subcapsular line signal corresponds
to the intracapsular tear. This sign is known as salad oil (foci of hypersignal on
T2 inside the prosthesis)24.
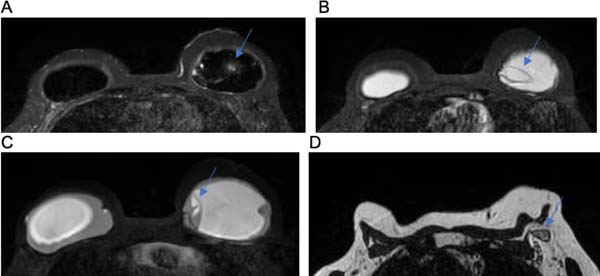
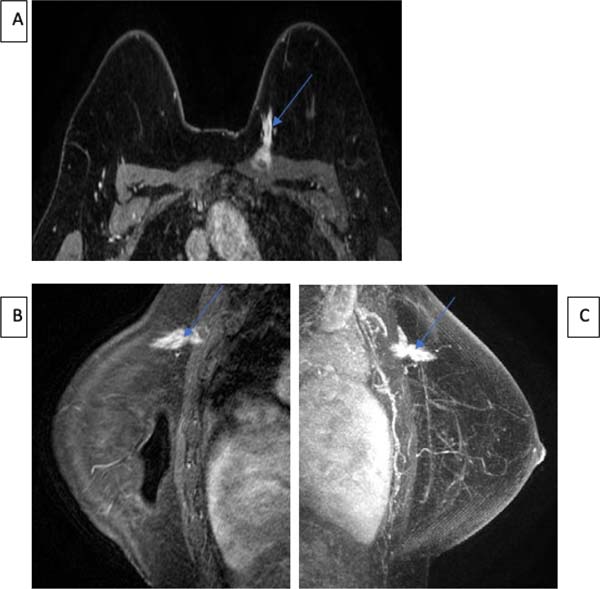
Two patients presented intracapsular rupture, as shown in Figure 8C, which depicts the linguine sign, and the presence of several hypointense curvilinear
lines within the silicone gel.
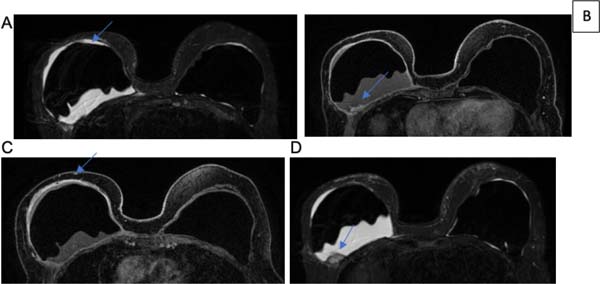
The radiological sign of capsular contracture shown in Figures 1C and 2D can be analyzed as an increase in the anteroposterior diameter of the implant, associated
with its asymmetry and rounded shape8.
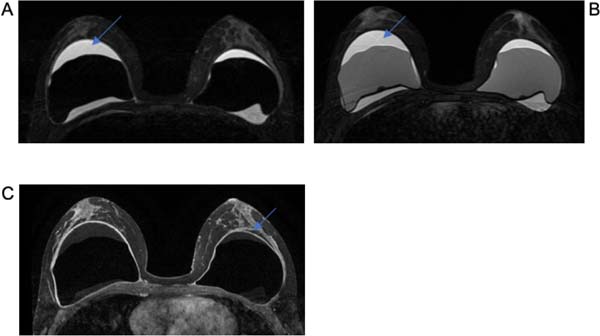
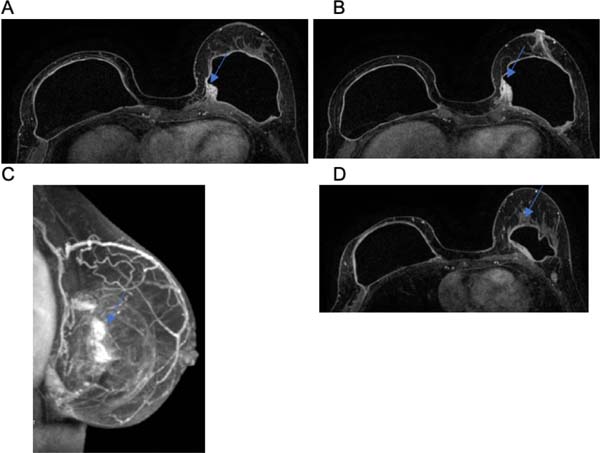
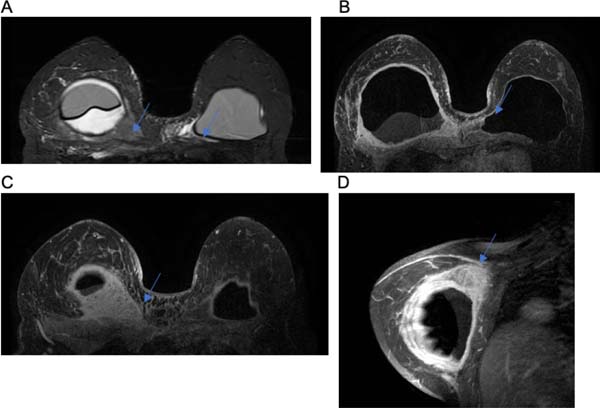
Figure 1 - A and B. Axial T2 sequences show a large bilateral pericapsular seroma, slightly larger
on the right. C. Post-contrast T1 sequence in axial plane showing slight thickening
and enhancement of the fibrous capsule (arrows).
Figure 1 - A and B. Axial T2 sequences show a large bilateral pericapsular seroma, slightly larger
on the right. C. Post-contrast T1 sequence in axial plane showing slight thickening
and enhancement of the fibrous capsule (arrows).
Large late seromas were found in group 1 and are exemplified in Figures 1A, 1B, 2A, and 3C. In the literature, possible etiological assumptions point to rupture of the prosthesis,
which did not occur in any case25. However, in prospective studies, it was estimated that BIA-ALCL occurs in 9 to 13%
of late seroma presentations17. But this fact could be justified by other causes, such as, for example, friction
between the prosthesis and the organic pocket, the chronic inflammatory process, and
metaplasia of the internal surface of the capsule10.
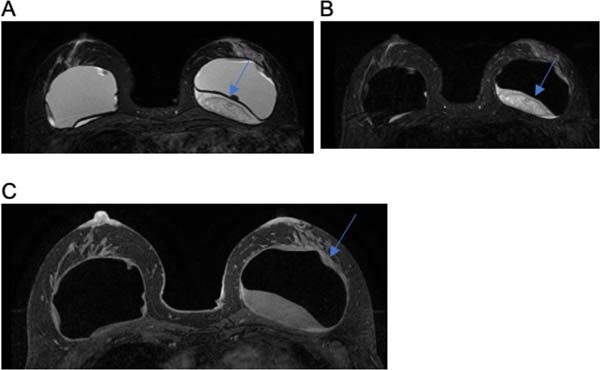
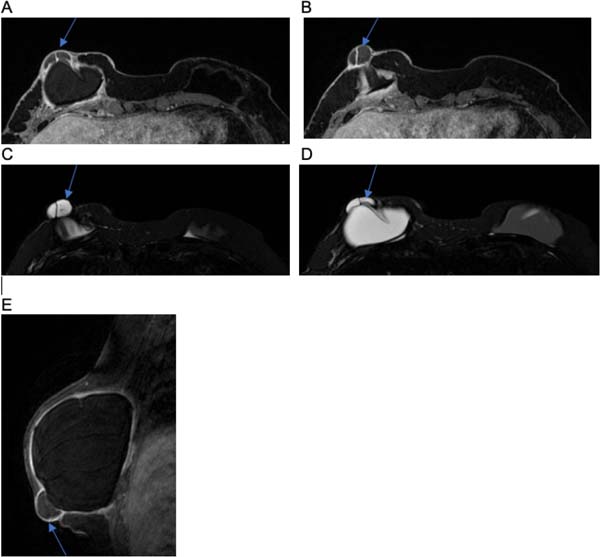
Figure 2 - A. Axial T2 sequence showing a large pericapsular seroma on the right, slightly hyperproteic.
B and C. Post-contrast T1 (B) and T2 (C) sequences in the axial plane show hyperintense
capsular nodular image on T2 and with heterogeneous and persistent enhancement on
the posterior aspect of the right implant, suggestive of induced silicone capsular
granuloma (arrows). D. Post-contrast T1 sequence in axial plane showing changes in
the morphology of the right implant, with a reduction in lobulations associated with
thickening and diffuse and irregular pericapsular enhancement, suggestive of capsular
contracture.
Figure 2 - A. Axial T2 sequence showing a large pericapsular seroma on the right, slightly hyperproteic.
B and C. Post-contrast T1 (B) and T2 (C) sequences in the axial plane show hyperintense
capsular nodular image on T2 and with heterogeneous and persistent enhancement on
the posterior aspect of the right implant, suggestive of induced silicone capsular
granuloma (arrows). D. Post-contrast T1 sequence in axial plane showing changes in
the morphology of the right implant, with a reduction in lobulations associated with
thickening and diffuse and irregular pericapsular enhancement, suggestive of capsular
contracture.
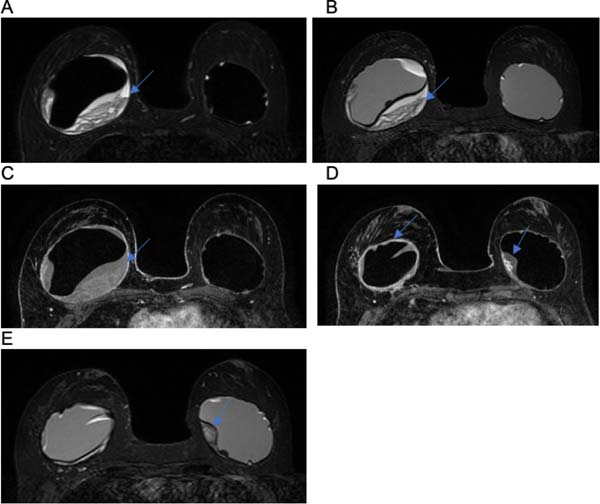
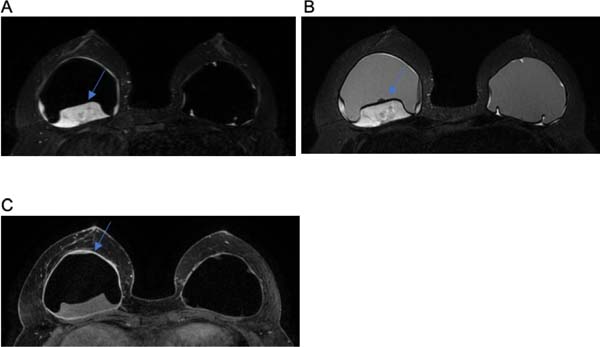
Figure 3 - A, B, and C. Post-contrast T2 (A and B) and T1 (C) sequences in the axial plane show
a large heterogeneous hyperproteic pericapsular seroma on the right and diffuse pericapsular
thickening and enhancement. D and E. Post-contrast T1 (D) and T2 (E) sequences in
the axial plane showing hyperintense capsular nodular image on T2 and with heterogeneous
and persistent enhancement in the left implant, suggestive of induced silicone capsular
granuloma (arrow).
Figure 3 - A, B, and C. Post-contrast T2 (A and B) and T1 (C) sequences in the axial plane show
a large heterogeneous hyperproteic pericapsular seroma on the right and diffuse pericapsular
thickening and enhancement. D and E. Post-contrast T1 (D) and T2 (E) sequences in
the axial plane showing hyperintense capsular nodular image on T2 and with heterogeneous
and persistent enhancement in the left implant, suggestive of induced silicone capsular
granuloma (arrow).
Pinchuk & Tymofii26, in a series of 569 patients who had breast implants, reported 6 cases of late seroma,
occurring between 2 years and 10 years postoperatively. In the authors’ opinion, the
friction of the prosthesis against the internal surface of the organic capsule was
one of the main reasons for synovial metaplasia on this surface, but also chronic
infection and the consequent formation of seroma.
Lymphatic drainage of the breast occurs mainly via 3 routes: supraclavicular, axillary,
and internal mammary, justifying the local lymphadenopathy in cases of prosthesis
rupture27, similar to what occurred in case 8 and demonstrated in Figure 8D. Silicone lymphadenopathy is an unusual finding on MRI and has a poorly understood
mechanism. However, it is believed that silicone particles are transported to lymph
nodes via macrophages in the reticuloendothelial system. In these cases, the diagnosis
of breast cancer must be excluded25.
Unlike rupture, silicone gel leakage is microscopic through an intact implant shell.
This phenomenon is related to the chemical affinity between the outer layer of the
silicone elastomer and the gel contained therein14. Contact with the outer shell can disrupt non-covalent molecular bonds between polymer
chains, causing swelling and weakening of the shell itself. Once separated from its
envelope, the silicone can migrate, reaching the upper limbs, inguinal lymph nodes,
and pleural fluid. Thus, the possible change in two patients in group 2 with axillary
lymph node disease and intra-node silicone can be explained. When gel extravasation
is extensive, it can be detected by imaging examination, resulting in the formation
of the inverted tear sign6,10.
Capsular granuloma was evident in two patients, as seen in Figures 2D, 4A and 4B. Furthermore, edema of the pectoral muscle was noted in one patient, as shown in
Figure 9A. The changes in question can be explained by the literature. In this case, the implant’s
silicone gel may have its envelope dissolved over time, making its coating thinner,
or even dissolved completely, which makes the product viscous inside the organic fibrous
capsule. Thus, in certain cases, there is migration of the viscous product to neighboring
tissues, which can form granulations, inflammation of the skin with skin rash, urticaria,
calcifications, migration to lymph nodes, or even infiltration into chest muscles,
simulating tumors25.
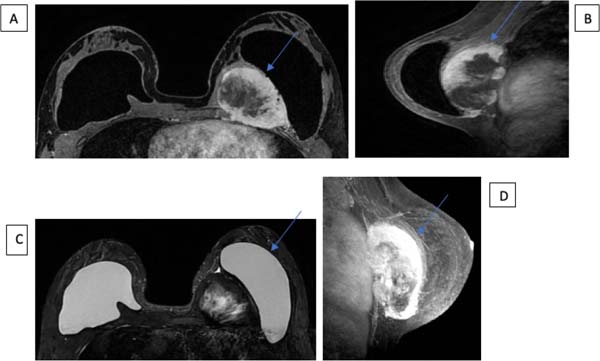
Figure 4 - A and B. Post-contrast T1 (A) and T2 (B) sequences in the axial plane showing hyperintense
capsular nodular image on T2 and with heterogeneous and persistent enhancement on
the left implant, suggestive of induced silicone capsular granuloma (arrow).
Figure 4 - A and B. Post-contrast T1 (A) and T2 (B) sequences in the axial plane showing hyperintense
capsular nodular image on T2 and with heterogeneous and persistent enhancement on
the left implant, suggestive of induced silicone capsular granuloma (arrow).
Figure 5 - A, B, and C. Post-contrast T1 sequences in the axial plane showing enhancement of
the breast parenchyma in the posterior third of the medial quadrants of the left breast,
next to the breast implant, associated with enhancement of the fibrous capsule and
local skin thickening and enhancement. D. 3D MIP reconstruction (maximum intensity
projection) in the sagittal plane demonstrating these findings.
Figure 5 - A, B, and C. Post-contrast T1 sequences in the axial plane showing enhancement of
the breast parenchyma in the posterior third of the medial quadrants of the left breast,
next to the breast implant, associated with enhancement of the fibrous capsule and
local skin thickening and enhancement. D. 3D MIP reconstruction (maximum intensity
projection) in the sagittal plane demonstrating these findings.
Figure 6 - A and B. Axial T2 sequences showing heterogeneous pericapsular seroma on the left
(arrows), in addition to reduced lobulations of this implant. C. Post-contrast T1
sequences in the axial plane showing thickening and diffuse enhancement of the fibrous
capsule of the left implant (arrow).
Figure 6 - A and B. Axial T2 sequences showing heterogeneous pericapsular seroma on the left
(arrows), in addition to reduced lobulations of this implant. C. Post-contrast T1
sequences in the axial plane showing thickening and diffuse enhancement of the fibrous
capsule of the left implant (arrow).
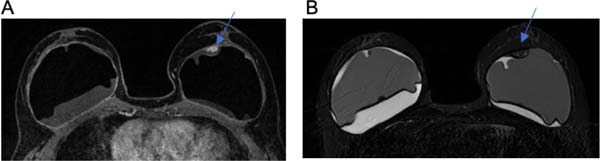
Figure 7 - A and B. Axial T2 sequences showing heterogeneous pericapsular seroma on the right
(arrows). C. Post-contrast T1 sequence in axial plane showing thickening and diffuse
enhancement of the fibrous capsule of the right implant (arrow).
Figure 7 - A and B. Axial T2 sequences showing heterogeneous pericapsular seroma on the right
(arrows). C. Post-contrast T1 sequence in axial plane showing thickening and diffuse
enhancement of the fibrous capsule of the right implant (arrow).
Figure 8 - A, B, and C. Axial T2 sequences showing tiny liquid inclusions in the left implant
(A and C) and “linguine sign” (B), suggestive of intracapsular rupture of the external
lumen. D. T1 sequence in axial plane showing left axillary lymph node enlargement,
with a heterogeneous signal similar to that of silicone (arrow), which may correspond
to intra-nodal silicone and suggest ipsilateral extracapsular rupture.
Figure 8 - A, B, and C. Axial T2 sequences showing tiny liquid inclusions in the left implant
(A and C) and “linguine sign” (B), suggestive of intracapsular rupture of the external
lumen. D. T1 sequence in axial plane showing left axillary lymph node enlargement,
with a heterogeneous signal similar to that of silicone (arrow), which may correspond
to intra-nodal silicone and suggest ipsilateral extracapsular rupture.
Figure 9 - A. T2 sequence in the axial plane showing loss of lobulations and rounded morphology
of the right implant, associated with a pericapsular seroma displacing this implant
anteriorly, in addition to diffuse edema of the underlying pectoral muscle (arrow)
and the medial aspect of the contralateral pectoral muscle (arrow). B, C, and D. Post-contrast
T1 sequences in axial (B and C) and sagittal planes (D) showing marked thickening
and irregular diffuse pericapsular enhancement of the right implant, especially in
its posterosuperior aspect (C and D - arrow), with pre-sternal extension towards the
fibrous capsule of the contralateral implant (B - arrow) and associated with thickening
and faint skin enhancement in the lower and medial quadrants of the right breast.
Figure 9 - A. T2 sequence in the axial plane showing loss of lobulations and rounded morphology
of the right implant, associated with a pericapsular seroma displacing this implant
anteriorly, in addition to diffuse edema of the underlying pectoral muscle (arrow)
and the medial aspect of the contralateral pectoral muscle (arrow). B, C, and D. Post-contrast
T1 sequences in axial (B and C) and sagittal planes (D) showing marked thickening
and irregular diffuse pericapsular enhancement of the right implant, especially in
its posterosuperior aspect (C and D - arrow), with pre-sternal extension towards the
fibrous capsule of the contralateral implant (B - arrow) and associated with thickening
and faint skin enhancement in the lower and medial quadrants of the right breast.
Figure 10 - Post-contrast T1 sequences in the axial plane (A and B) and T2 sequences in the axial
plane (C and D) showing herniation of the fibrous capsule with heterogeneous content
in the inferolateral quadrant of the right breast (arrows). E. Post-contrast T1 sequence
in sagittal plane showing the subcutaneous location of the herniation, in close contact
with the skin (arrow).
Figure 10 - Post-contrast T1 sequences in the axial plane (A and B) and T2 sequences in the axial
plane (C and D) showing herniation of the fibrous capsule with heterogeneous content
in the inferolateral quadrant of the right breast (arrows). E. Post-contrast T1 sequence
in sagittal plane showing the subcutaneous location of the herniation, in close contact
with the skin (arrow).
Figure 11 - In the topography of the left pectoral muscle, in its central and medial aspects,
at the level of the second to fifth intercostal spaces, there is a heterogeneous solid-cystic
nodular image, with irregular thick walls and heterogeneous enhancement, measuring
9.4 x 7.2 x 5.0 cm, with rapid initial enhancement and persistent type kinetic curve.
This nodular image displays intimate contact with the implant capsule (with its enhancement
and displacing the implant anteriorly) and also displays contiguity with the intercostal
muscles posteriorly (with its enhancement), attached to the pulmonary pleura and pericardium
in the respective intercostal spaces and without enhancement of the adjacent costal
arches and cartilages.
Figure 11 - In the topography of the left pectoral muscle, in its central and medial aspects,
at the level of the second to fifth intercostal spaces, there is a heterogeneous solid-cystic
nodular image, with irregular thick walls and heterogeneous enhancement, measuring
9.4 x 7.2 x 5.0 cm, with rapid initial enhancement and persistent type kinetic curve.
This nodular image displays intimate contact with the implant capsule (with its enhancement
and displacing the implant anteriorly) and also displays contiguity with the intercostal
muscles posteriorly (with its enhancement), attached to the pulmonary pleura and pericardium
in the respective intercostal spaces and without enhancement of the adjacent costal
arches and cartilages.
Figure 12 - In the superomedial quadrant of the left breast, 11 o’clock, posterior third, close
to the presternal region, there is nodular, irregular, spiculated, heterogeneous enhancement,
measuring 3.4 x 3.2 x 2.2 cm, 9.7 cm away from the nipple-areola complex and invading
the anterior half of the ipsilateral pectoral muscles, with rapid initial enhancement
and persistent type kinetic curve.
Figure 12 - In the superomedial quadrant of the left breast, 11 o’clock, posterior third, close
to the presternal region, there is nodular, irregular, spiculated, heterogeneous enhancement,
measuring 3.4 x 3.2 x 2.2 cm, 9.7 cm away from the nipple-areola complex and invading
the anterior half of the ipsilateral pectoral muscles, with rapid initial enhancement
and persistent type kinetic curve.
Desmoid fibromatosis (DF) is a non-metastatic, rare, locally aggressive myofibroblastic
tumor, with high recurrence rates (24-77%) and an unpredictable clinical course. The
incidence is approximately 0.2% of all breast neoplasms28. The most affected site is intra-abdominal, with the breast being an extremely rare
condition29. Two patients were found in whom the hypothesis of malignant breast tumor was initially
raised, which the biopsy and immunohistochemistry results confirmed to be a desmoid
tumor. In immunohistochemistry, the positive presence of actin and vimentin, desmin
is rarely positive, while S100 and CD34 are negative, being useful for the diagnosis
of desmoid tumor29.
On MRI, desmoid tumors are typically irregular masses, with a poorly defined contour,
hypointense, and isointense concerning the muscle in T1-weighted sequences and with
variable signal hyperintensity in T230-weighted sequences. These findings are evidenced
in Figures 11A, 11B, 12A and 12B.
Diagnostic investigation through imaging tests such as magnetic resonance imaging
can facilitate the elucidation of so-called “unusual” complications in breast implant
surgeries. Given these possible changes, the patient must be informed in advance about
the inclusion of breast implants, as her decision may have future implications, requiring
new surgical interventions for treatment if complications occur.
CONCLUSION
It is estimated that there are 50 million women with breast implants in the world.
The number of women undergoing breast augmentation with silicone implants tends to
increase and Brazil is one of the main countries in statistical numbers. Based on
this trend, the number of so-called “unusual” complications becomes a diagnostic challenge
for plastic surgeons and radiologists.
In the present study, a low incidence of unusual complications was found, with 12
cases out of 211 analyzed using breast MRI. This diagnostic method helps in the early
detection of these changes and provides greater safety for post-operative monitoring,
due to its high sensitivity and specificity, playing a central role in therapeutic
guidance.
REFERENCES
1. Baker JL Jr, Kolin IS, Bartlett ES. Psychosexual dynamics of patients undergoing mammary
augmentation. Plast Reconstr Surg. 1974;53(6):652-9.
2. Pitanguy I, Barbato C, Dègand M, Lopez CET. Mamoplastia de aumento: considerações
sobre a retração capsular. Rev Bras Cir. 1979;69(7/8):237-50.
3. Montandon RE. A report on complications of breast implantation: evaluation of 546
cases in 8 years. Rev Bras Cir Plást. 2014;29(3):352-60.
4. Pitanguy I, Amorim NFG, Ferreira AV, Berger R. Análise das trocas de implantes mamários
nos últimos cinco anos na clínica Ivo Pitanguy. Rev Bras Cir. 2010;25(4):668-74.
5. Gorczyca DP, Gorczyca SM, Gorczyca KL. The diagnosis of silicone breast implant rupture.
Plast Reconstr Surg. 2007;120(7 Suppl 1):49S-61S.
6. Dancey A, Nassimizadeh A, Levick P. Capsular contracture - What are the risk factors?
A 14 year series of 1400 consecutive augmentations. J Plast Reconstr Aesthet Surg.
2012;65(2):213-8.
7. McGrath MH, Burkhardt BR. The safety and efficacy of breast implants for augmentation
mammaplasty. Plast Reconstr Surg. 1984;74(4):550-60.
8. Wiedenhoefer JF, Shahid H, Dornbluth C, Otto P, Kist K. MR imaging of breast implants:
useful information for the interpreting radiologist. Appl Radiol. 2015;44(10):18-24.
9. Sperli A, Bersou Jr. A, Freitas JOG, Michalany N. Complicações com Próteses Mamárias.
Rev Bras Cir Plást. 2000;15(3):33-46.
10. Franco T, Franco D. Seroma tardio após implantes mamários de silicone: três formas
diferentes de apresentação, evolução e conduta. Rev Bras Cir Plást. 2013;28(2):247-52.
11. Nahabedian MY, Patel K. Management of common and uncommon problems after primary breast
augmentation. Clin Plast Surg. 2009;36(1):127-38.
12. Biggs TM, Cukier J, Worthing LF. Augmentation mammaplasty: a review of 18 years. Plast
Reconstr Surg. 1982;69(3):445-52.
13. De Cholnoky T. Augmentation mammaplasty. Survey of complications in 10,941 patients
by 265 surgeons. Plast Reconstr Surg. 1970;45(6):573-7.
14. Colombo G, Ruvolo V, Stifanese R, Perillo M, Garlaschi A. A. Prosthetic breast implant
rupture: imaging--pictorial essay. Aesthetic Plast Surg. 2011;35(5):891-900.
15. Seiler SJ, Sharma PB, Hayes JC, Ganti R, Mootz AR, Eads ED, et al. Multimodality Imaging-based
Evaluation of Single-Lumen Silicone Breast Implants for Rupture. Radiographics. 2017;37(2):366-82.
16. Barra RF, Barra RR, Barra Sobrinho A. Novos métodos funcionais na avaliação de lesões
mamárias. Radiol Bras. 2012;45(6):340-4.
17. Cordeiro PG, Ghione P, Ni A, Hu Q, Ganesan N, Galasso N, et al. Risk of breast implant
associated anaplastic large cell lymphoma (BIA-ALCL) in a cohort of 3546 women prospectively
followed long term after reconstruction with textured breast implants. J Plast Reconstr
Aesthet Surg. 2020;73(5):841-6.
18. Argus A, Mahoney MC. Indications for breast MRI: case-based review. AJR Am J Roentgenol.
2011;196(3 Suppl):WS1-14.
19. De-Azambuja AP, Groth AK, Jung J, Gevert F, Nabhan SK. Breast implant-associated anaplastic
large cell lymphoma: a diagnostic challenge. Rev Bras Cir Plást. 2020;35(1):118-20.
20. Juanpere S, Perez E, Huc O, Motos N, Pont J, Pedraza S. Imaging of breast implants-a
pictorial review. Insights Imaging. 2011;2(6):653-70.
21. Stöblen F, Rezai M, Kümmel S. Imaging in patients with breast implants-results of
the First International Breast (Implant) Conference 2009. Insights Imaging. 2010;1(2):93-7.
22. Yang N, Muradali D. The augmented breast: a pictorial review of the abnormal and unusual.
AJR Am J Roentgenol. 2011;196(4):W451-60.
23. Soo MS, Kornguth PJ, Walsh R, Elenberger C, Georgiade GS, DeLong D, et al. Intracapsular
implant rupture: MR findings of incomplete shell collapse. J Magn Reson Imaging. 1997;7(4):724-30.
24. Schmitt W, Coelho JM, Lopes J, Marques JC. O Papel da Radiologia na Monitorização
das Complicações Relacionadas com as Próteses Mamárias. Acta Radiol Port. 2018;30(1):23-34.
25. Takejima AL. Ruptura de implante mamário com disseminação linfática do silicone: relato
de caso e revisão da literatura [Trabalho de Conclusão de Curso em Residência Médica].
São Paulo: Hospital do Servidor Público Municipal; 2011.
26. Pinchuk V, Tymofii O. Seroma as a late complication after breast augmentation. Aesthetic
Plast Surg. 2011;35(3):303-14.
27. Moore KL, Daley AF. Anatomia orientada para a clínica. 7ª ed. Rio de Janeiro: Guanabara
Koogan; 2014.
28. Benej R, Mečiarová I, Pohlodek K. Desmoid-type fibromatosis of the breast: A report
of 2 cases. Oncol Lett. 2017;14(2):1433-8. DOI: 10.3892/ol.2017.6337
29. Duazo-Cassin L, Le Guellec S, Lusque A, Chantalat E, Laé M, Terrier P, et al. Breast
desmoid tumor management in France: toward a new strategy. Breast Cancer Res Treat.
2019;176(2):329-35. DOI: 10.1007/s10549-019-05245-5
30. Erguvan-Dogan B, Dempsey PJ, Ayyar G, Gilcrease MZ. Primary desmoid tumor (extraabdominal
fibromatosis) of the breast. AJR Am J Roentgenol. 2005;185(2):488-9.
1. Hospital Daher Lago Sul, Brasília, DF, Brazil
Corresponding author: Igor Moura Soares Quadra SHIS QI 7, conjunto F, área especial F, Setor de Habitações Individuais Sul,
Brasília, DF, Brazil, Zip Code: 71615-660, E-mail: igormoura739@gmail.com
Article received: January 19, 2024.
Article accepted: February 4, 2024.
Conflicts of interest: none.