INTRODUCTION
The mandible is the largest and strongest of the facial bones, presenting itself as
a primordial structure in basic routine functions such as chewing, phonation, and
swallowing1. Due to its topography, anatomy, projection in the lower third of the face, and motility
concerning the skull base, the mandible is more vulnerable to external trauma, appearing
in statistics as one of the most commonly fractured bones2,3. Classically, we found a patient complaining of pain, edema, hematoma, unsatisfactory
dental occlusion, alteration of facial contour, crackling, and mobility of bone fragments4 in mandibular fractures. The main objective of treating mandibular fractures is to
restore dental occlusion and masticatory function.
According to data from the Hospital Information System of the Unified Health System,
in 2019, 142,800 deaths from external causes were recorded5. Trauma consists of sudden injuries caused by external forces, such as car accidents
or assaults.
Among the most commonly identified physical traumas, skull and face fractures - isolated
or associated with polytrauma - are observed daily in emergency hospitals and may
correspond to approximately 50% of all deaths from traumatic causes6. Their consequences constitute a major challenge for the health system since they
are responsible for most permanent disabilities, generating a great demand for access,
resources, and specialized urgent and emergency services7.
Because it has heterogeneous epidemiological aspects, the collection and analysis
of demographic data on mandible fractures are fundamental to assist in the management
of patients, in addition to helping to create health promotion programs and preventive
campaigns. Because of the relative frequency of this type of fracture in trauma centers,
as well as due to sociocultural changes, represented in this context mainly by an
increase in interpersonal violence and car traffic, this work intends to outline the
epidemiological profile of patients treated at a referenced Emergency Care from a
teaching hospital in Campinas, in the state of São Paulo, between April 2015 and April
2020.
OBJECTIVE
To carry out an epidemiological and topographical survey of traumas diagnosed with
mandibular fractures that were surgically treated among patients at a university hospital.
METHOD
A retrospective epidemiological study was carried out at the Hospital de Clínicas
da UNICAMP (HC-UNICAMP), located in the city of Campinas, in the state of São Paulo,
characterized as a university hospital, between April 1, 2015 and April 1, 2020.
The initial selection of which patients would be analyzed to determine the epidemiological
profile of mandibular fractures undergoing surgical procedures was carried out using
the HC-UNICAMP surgery database in a report provided by the institution’s information
system team. Once all surgeries for correction of mandible fractures were identified
in the period mentioned above, the medical records of each patient included in the
study were consulted.
Data was collected by two plastic surgery residents and a medical student, with the
entire team trained to tabulate data in a standardized way.
Only patients who had a medical record related to a mandibular fracture were included
in the study, including information on the etiology of the trauma, sex, age, topography
of the fractures, comorbidities, treatment instituted, need for an Intensive Care
Unit (ICU) at some point during the treatment, surgeries with other specialties and
surgical complications.
Data were submitted to descriptive and quantitative analyses, represented by means,
medians, and percentages.
This study applied the Informed Consent Form (ICF) to all patients who were still
being followed up at the Plastic Surgery outpatient clinic at HC-UNICAMP and those
who were located for an appointment via telephone contact. A consent form was waived
for the patient no longer undergoing outpatient follow-up of the fracture correction
surgery, who eventually died, or with whom it was impossible to contact.
All information collected was treated with absolute secrecy by the researchers, and
data collection was started only after approval of the research project by the Research
Ethics Committee via Plataforma Brasil, CAAE: 42733320.1.0000.5404.
RESULTS
We identified 53 patients who underwent surgical treatment for a mandible fracture
between April 2015 and April 2020. Three participants were excluded from the study
for having incomplete medical records. Fifty patients were included, and in 98% (n=49)
of the cases, rigid internal fixation with miniplates and screws was used, and only
one patient had the sequelae of a mandible fracture treated through orthognathic surgery.
Antibiotic prophylaxis was performed in all surgeries. Postoperatively, patients were
instructed to eat a liquid and pasty diet for at least two weeks to maintain strict
oral hygiene with toothbrushing, mouthwashes with chlorhexidine, and applying cold
compresses to the face.
Most patients were male (n=45, 90%), with only 10% (n=5) female. The mean age was
30.7 years (the extremes of age: 10 and 63 years), with a median of 29.5 years. Thirty-four
(68%) of the patients declared themselves white, 15 (30%) brown, and 1 (2%) black.
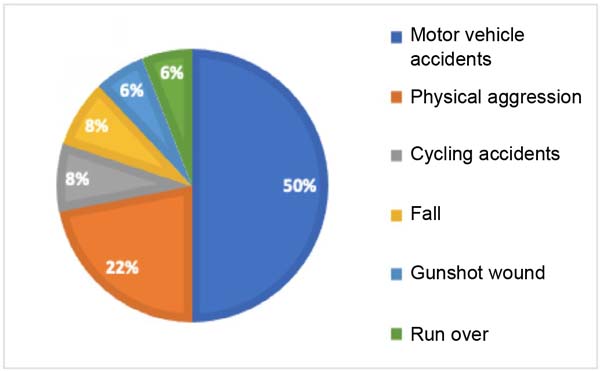
As for the etiology of the trauma, 25 (50%) suffered accidents while occupied motor
vehicles (motorcycles, cars, trucks), 11 (22%) were victims of physical aggression,
4 (8%) had accidents with bicycles, the same number found in falls (n=4, 8%), 3 (6%)
fractured the mandible in gunshot wounds, the same percentage measured in pedestrian
accidents (n=3, 6%), as shown in Figure 1.
Figure 1 - Etiology of trauma.
Figure 1 - Etiology of trauma.
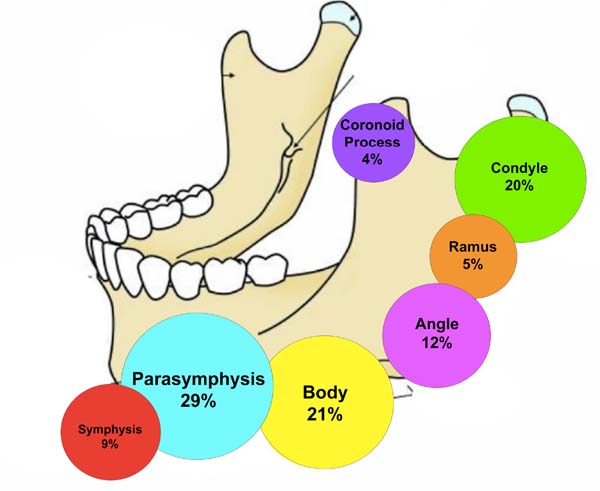
In the analysis of the CT scans of the face performed, we found that 29 (58%) patients
had fractures in more than one mandibular region, totaling 92 fractures in the 50
patients studied. Figure 2 shows the topography of the lesions, with the parasymphysis being the most fractured
structure (27/92, 29%), followed by the body (19/92, 21%), condyle (18/92, 20%), angle
(11/92, 12%), symphysis (8/92, 9%), ramus (5/92, 5%) and the least affected the coronoid
process (4/92, 4%).
Figure 2 - Topography of mandible fractures.
Figure 2 - Topography of mandible fractures.
The median time between trauma and surgery was 19 days, ranging from 0 to 412 days.
The prolonged time is due to a single patient case later submitted to sequel treatment.
Eleven (22%) patients had some comorbidity, with the use of psychoactive substances
being the highlight: 12% (6) were smokers, 6% (3) alcoholics, 2% (1) illicit drugs.
Ten (20%) patients had some complication of the surgery, the most common being surgical
wound dehiscence (4.8%), plaque extrusion (3.6%), followed by surgical wound infection,
thread granuloma and fistula of the palate, 2% each of them respectively. Surgical
reapproach was necessary in 14% (7) of the patients due to complications, with removal
of the fixation plate being the most commonly performed surgery.
Fourteen patients (28%) were admitted to the ICU, with the median and average length
of stay being 12 days. Twenty-one (42%) operated with another specialty in addition
to plastic surgery, with orthopedics responsible for the approach to 28% of these
patients, followed by trauma surgery in 16% of cases and neurosurgery in 6% of cases.
DISCUSSION
Mandible fracture is one of the most prevalent among facial bones4,8-10. Since it is involved in mastication, speech, and swallowing, injuries to its apparatus
can lead to important anatomical and functional damage, impairing the patient’s quality
of life1.
In this study, most patients were treated with rigid internal fixation with titanium
miniplates, which restores the union of fractured and displaced foci, giving them
stability and offering early functional recovery since it allows early mobility of
the mandible1,11. A few years ago, the use of maxillomandibular block was predominant as a treatment
for this type of fracture; however, there was a transition in surgeons’ preference
for open reduction and rigid internal fixation with miniplate and titanium screw.
Some factors that contributed to the change were the increase in body and angle fractures,
often classified as unfavorable, a higher prevalence of edentulous patients in large
urban centers, and a higher incidence of multiple fractures12. We use maxillomandibular locking at the time of osteosynthesis with miniplates and
sometimes for a short period in the postoperative period in cases of complex fractures,
as it allows greater stability to the fracture foci.
There is agreement between many of the studies on mandible fractures concerning the
predominance of occurrence in young males1,4,6,11,13,14. This can be explained by the fact that this population is exposed to driving on
highways, in sports activities, and in bars, making greater use of alcohol and psychoactive
substances and, consequently, being involved in a higher incidence of trauma1,11.
However, it is worth highlighting the increasing number of facial traumas in women
in recent decades, related to behavioral changes and greater participation of women
in society15. The mean age of the patients was 30.7 years, slightly higher than that found in
other national studies; however, compared with the age found in our median of 29.5,
the data are very similar1,4,11,12 ,14,16.
It is important to emphasize the economic impact of this scenario since this productive
population is temporarily removed from their jobs. Concerning color, the percentages
found in this study were similar to those computed by the 2010 Census, when 63.9%
of São Paulo inhabitants declared themselves white, 29.1% brown, 5.5% black, 1.4%
yellow, and 0.1% indigenous17.
The cause of the fracture has an extremely variable incidence depending on social,
geographic, and economic characteristics. Due to the current epidemiological profile
of morbidity and mortality, there is a predominance of fractures caused by traffic
accidents and violence, which is fundamentally urban4. This series’s most frequent etiological factor was related to motor vehicle accidents,
consistent with several other studies1,4,11,18. However, a progressive trend in the incidence of cases of physical aggression can
be observed in the literature12,16. This fact reflects the increase in violence and unemployment in cities and, on the
other hand, the establishment of stricter traffic laws, with higher fines and greater
acceptance of using seat belts12,18.
In the analysis of the computed tomography of the face, we found that
29 (58%) patients had multiple mandibular fractures, a higher number than reported
by other groups in Brazil1,4. This finding can be explained by the care for more complex traumas, such as car
accidents and falls from great heights in our service.
The location of the mandible fracture is variable, depending on the etiology of the
trauma, which explains the fact that the literature is very divergent regarding the
most affected sites11. Most studies revealed a greater involvement of the regions of the body, symphysis,
and mandibular condyles1,11,13,19, followed by angle trauma and mandibular ramus, respectively11,19. In our study, the predominant fracture site was the parasymphysis, as in a study
conducted in Ceará11. Symphysis and parasymphysis fractures were also the most common in a study conducted
in Singapore, representing 46.5% of cases20.
Since most victims are young, it is common for them to be healthy; however, it is
important to emphasize that 20% of our casuistry uses psychoactive substances. Several
studies associate the occurrence of facial fractures with the ingestion of alcoholic
beverages1,4.
The time elapsed between the trauma and the reduction and fixation of the mandible
was prolonged compared to other studies1,4,13. It is known that mandible fractures in car occupants are related to accidents with
a higher amount of energy18. Because of this, patients commonly had prolonged hospitalization due to the severity
of the condition, with the need for admission to the ICU and surgical intervention
by other specialties, causing the surgery for facial fractures to be postponed until
the clinical condition stabilized or even until it was later treated as a sequel.
Our general rate of complications was 20%, slightly higher than that found in the
national literature, which varies between 10% and 18.6%1,4,12,21. This study differed from others published in the country, as the most common complication
was surgical wound dehiscence, while, commonly, infection is the most prominent finding.
Our infection rates, 2%, were lower than those of other national studies, which varied
between 6.1% and 9.6%1,4,12.
The high rates of ICU admissions, associated injuries, and surgical procedures carried
out by other specialties demonstrate the challenging scenario of trauma treated at
the service. The earlier the intervention, the lower the chances of greater complexity
in surgical procedures of greater complexity of surgical procedures due to fibrosis,
pseudarthrosis, overriding with calcification, and poor anatomical positioning of
the structures involved, possibly contributing to the percentage of complications
found16.
CONCLUSION
Mandible fractures were significantly more diagnosed in young males, with motor vehicle
accidents being the most prevalent cause. The main affected topographies were parasymphysis
and body, while the most frequent complication was surgical wound dehiscence. The
high rates of ICU admissions, associated injuries, and surgical procedures carried
out by other specialties demonstrate the challenging scenario of trauma treated at
our service.
1. Universidade Estadual de Campinas, Departamento de Cirurgia, Campinas, SP, Brazil
Corresponding author: Luiz Henrique Zanata Pinheiro Cidade Universitária Zeferino Vaz, Barão Geraldo, Campinas, SP, Brazil, Zip Code:
13083-970, E-mail: henriquez_pinheiro@hotmail.com