INTRODUCTION
Lips play a fundamental role in people’s daily lives, performing motor functions (facial
mimicry, speech articulation, and swallowing) and aesthetic importance, as they represent
one of the dynamic centers of the face and significantly impact an individual’s self-esteem
and quality of life1.
The main causes of lip deformities result from congenital malformations (cleft lip),
trauma, or loss of substance after resection of tumors in this region2.
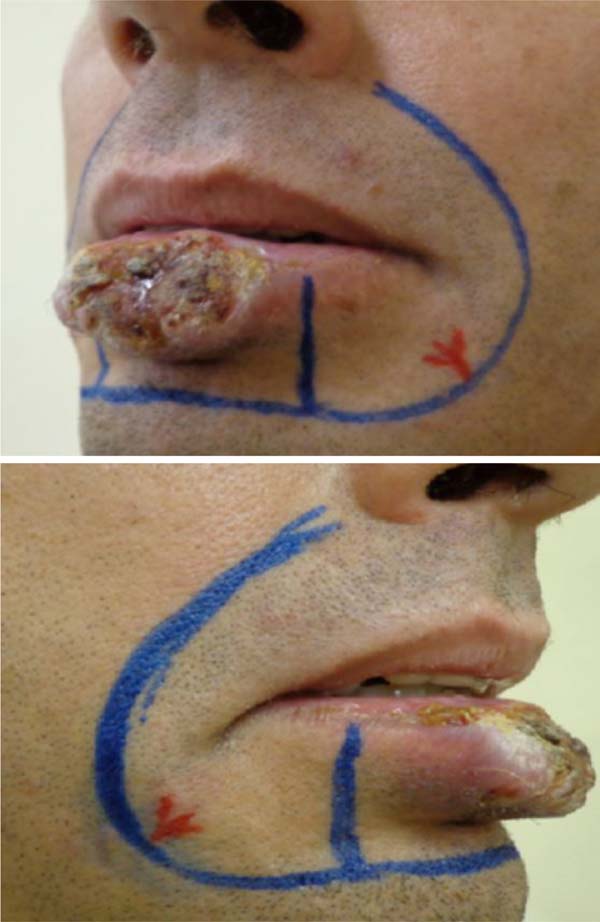
Squamous cell carcinoma (SCC) is the most common malignant tumor of the lips, being
most diagnosed on the lower lip3 (Figure 1), and accounts for approximately 25% to 30% of all types of oral cancer. The initial
clinical manifestations are atrophy, dryness, and fissures of the lip’s vermilion
with an undefined margin between the vermilion and the skin.
Figure 1 - Squamous cell carcinoma of the lower lip.
Figure 1 - Squamous cell carcinoma of the lower lip.
They mainly affect patients between 50 and 70 years of age, with males being preferential
compared to females4. This fact can be explained because men carry out outdoor activities (mainly outdoor
workers) and are more exposed to factors predisposing to lip cancer. It is known that
a large part of the male public, compared to the female, tends not to be concerned
about protecting themselves against solar radiation, such as lip balm5,6. SCC of the lips has some harmful practices as its main risk factors, such as long-term
sun exposure, alcohol consumption, smoking, and genetic predisposition5.
Adequate treatment of this neoplasm must be early and radical, as metastases can occur.
The doctor must always be prepared to conduct a meticulous intra and extraoral examination,
evaluating any change in normality. Once diagnosed and treated in its initial stage,
the progression of the injury can be prevented, establishing immediate treatment and
seeking to improve quality of life7. Traditional methods of cancer treatment are surgery, radiotherapy, and chemotherapy.
The treatment to be established will depend on the location, degree of malignancy,
tumor staging, and the individual’s health condition8.
Lip reconstruction aims to recover the functional aspect while maintaining the sphincter
component, seeking maximum preservation of sensitivity and oral opening with a satisfactory
aesthetic result. In order to obtain a good result in reconstruction, the following
principles must be respected: prioritize function over aesthetics, have local tissue
as the first option, reconstitute all damaged planes, and respect aesthetic units1.
Surgical resection with safe margins is the treatment of choice, whenever possible,
in the initial approach to SCC of the lower lip. In this context, Gillies was one
of the first to describe a technique, in 1920, to transpose the skin and nasolabial
mucosa to the lower lip through what he called a fan flap8,9.
This technique was later improved by Gillies and Millard in 195710, and again in 1974, with the description of the Karapandzic11 technique, which is a neurovascular myocutaneous flap that preserves labial vascularization
and innervation, requiring careful dissection that does not section the structures
vascular and nervous structures, preserving the sensation and motricity of the reconstructed
lip. The advantage of this technique is that it is a single-stage surgery, unlike
the Abbe flap12, with the ability to preserve both functionality and lip aesthetics.
The Karapandzic flap is an easy-to-perform technique that provides excellent results:
a lip with sensation and orbicularis function preserved from the first postoperative
day. Oral stoma reduction rarely causes significant problems, and the aesthetic result
is excellent because the scars are well positioned, the mouth is symmetrical, and
the nasolabial folds do not change. There is no evidence of flap bulging, and long-term
results reveal little chance of surgical reintervention; this is where the highlight
of this procedure lies, followed closely by the ease with which it is performed7.
Microstomia stands out among the Karapandzic technique’s main disadvantages, especially
when reconstructing larger defects13,14. Any injury that directly or indirectly affects the corners of the lips can lead
to microstomies (reduction in mouth opening), sometimes serious, with aesthetic and
functional impairments (eating, speech, and oral hygiene). Depending on the severity,
they require surgical and/or multidisciplinary treatment (dentist, speech therapist)15.
Anatomical considerations
Knowledge of the anatomy of the lip was necessary to indicate the appropriate technique
for reconstruction. The circular or semicircular fibers of the orbicularis oris muscle
and mentalis muscle represent the labial sphincter component (closure). The dilator
component (opening) is formed by the radial fibers of the facial muscles: levator
labii superioris and ala nasi, levator labii superioris, zygomaticus major, buccinator,
depressor anguli oris, depressor labii inferior, levator anguli oris. Irrigation is
provided by the superior and inferior labial arteries, branches of the facial artery.
Lymph drains into the submandibular and submental lymph nodes. The infraorbital nerve
provides the sensory innervation of the upper lip, the lower lip through the mental
nerve, and the motor through the facial nerve16.
Surgical technique
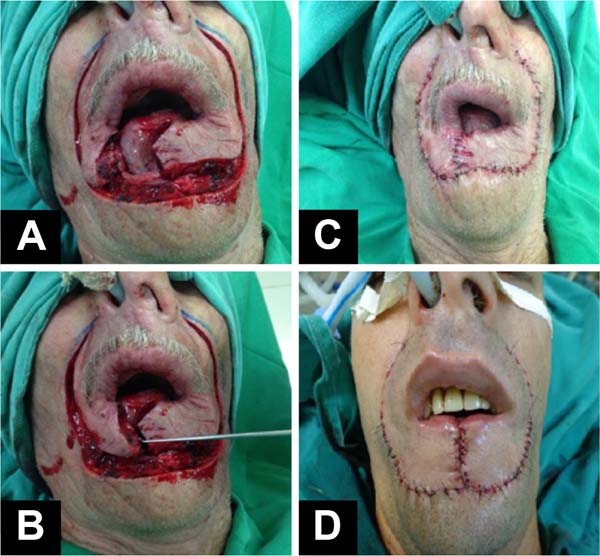
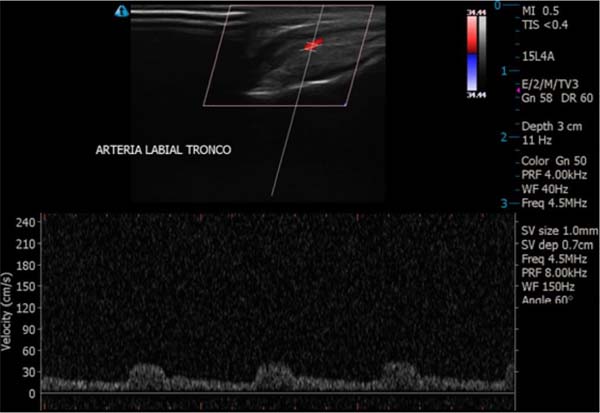
Patients were positioned in the supine position. Markings were made of the tumor area
to be resected, the flap lines, and the location of the neurovascular pedicle with
the aid of a portable echoDoppler (Figure 2). Subjected to general anesthesia and nasotracheal intubation, antisepsis with 4%
chlorhexidine digluconate and asepsis. Local anesthetic infiltration was performed
with a 0.5% bupivacaine solution containing vasoconstrictor - adrenaline at 1:200,000.
The squamous cell carcinoma was resected with minimum surgical margins of 4mm and
hemostasis (Figure 3).
Figure 2 - Preoperative marking on the skin (in red) of the vascular pedicles.
Figure 2 - Preoperative marking on the skin (in red) of the vascular pedicles.
Figure 3 - A: Markings of the flap lines and the lip resection area. B: Defect after tumor resection.
Figure 3 - A: Markings of the flap lines and the lip resection area. B: Defect after tumor resection.
The creation of the flaps was the next step: incision in the right and left nasolabial
line, careful dissection of the orbicularis muscle, identification, and preservation
of the arterial and venous (upper and lower labial) and nervous branches, obtaining
two myocutaneous flaps: right and left. Revision of hemostasis with a bipolar electric
scalpel and rotation of the flaps towards the midline. Synthesis of the muscles and
mucosa with simple, separate, and inverted sutures with absorbable 4.0 poliglecaprone
suture and suture of the skin with 5.0 and 6.0 monofilament nylon threads (Figure 4). Sterile adhesive dressing (Opsite®) was applied to the wound for the first 48 hours.
No drains were used.
Figure 4 - A and B: Creation and rotation of the myocutaneous flaps. C and D: Summary and appearance at the end of surgery.
Figure 4 - A and B: Creation and rotation of the myocutaneous flaps. C and D: Summary and appearance at the end of surgery.
OBJECTIVE
To demonstrate a reliable and safe option for lower lip reconstruction after excision
of squamous cell carcinoma using the Karapandzic technique.
METHOD
A cross-sectional, retrospective, descriptive, and observational study was carried
out on patients evaluated and operated on by the main author in the city of Barbacena-MG
from June 2013 to January 2022.
The study was approved by the Medical Ethics Committee of the service where it was
carried out (CEP approval number: 0001-2022), and the patients signed an Informed
Consent Form, including authorization for the dissemination of images for academic
purposes. Data was collected by analyzing the electronic medical records of patients
operated on by the same plastic surgeon and in the same service. The medical records
with “Lower Lip Reconstruction” or “Karapandzic Flap” were collected.
The inclusion criteria for this study were complete medical records, good-quality
photographic records, and patients with a minimum postoperative follow-up of 3 months.
Exclusion criteria include incomplete medical records, poor quality or missing photographs,
patients who did not receive proper postoperative follow-up, and/or patients operated
on by another surgeon.
During the period above, 4 patients underwent surgery. All males and evaluated preoperatively
with physical and laboratory examinations associated with lip Doppler ultrasound.
To identify the superior and inferior labial arteriovenous pedicles, a Mindray M7
portable color Doppler was used by the imaging specialist (Figure 5).
Figure 5 - Mindray M7 portable color ecoDoppler device.
Figure 5 - Mindray M7 portable color ecoDoppler device.
The images analyzed on the device screen in the immediate preoperative period, in
the operating room, attest to the viability of the pedicle bilaterally and the location
of this pedicle (Figure 6). In addition to checking the viability of the pedicle, marking the correspondence
of the arteriovenous bundle on the skin reduces the chances of partial or total perioperative
injury to this pedicle.
Figure 6 - Visualization of the vascular pedicle using the color echoDoppler device.
Figure 6 - Visualization of the vascular pedicle using the color echoDoppler device.
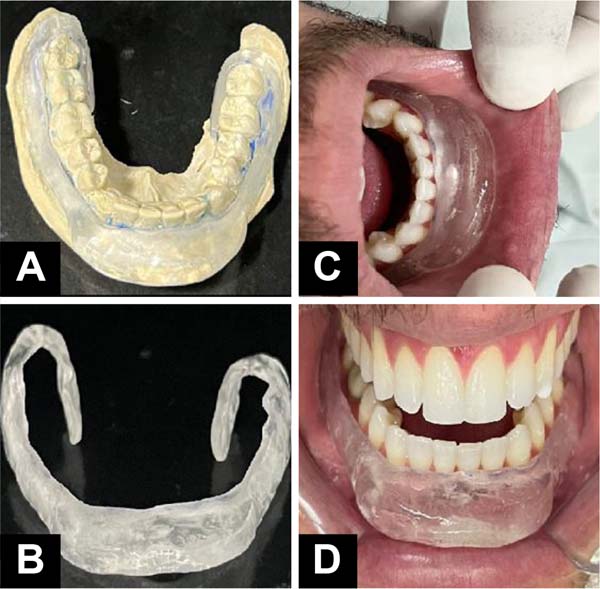
Patients who presented postoperative microstomia were referred to the orthodontist,
who created a static orthosis for nighttime use and of an individualized size and
specific for tissue expansion. The orthosis used was produced from an alginate mold,
then cast in type 2 stone plaster and sent to the dentistry laboratory, which makes
the orthosis using an acrylic plate and a metal base supported on the vestibular region
of the lower anterior teeth (Figure 7). Expansion sessions begin 60 days after surgery and are performed every 21 or 30
days, adding more polymerizable acrylic to the acrylic plate (Figure 8).
Figure 7 - A: Mold of the orthosis in alginate plate. B: Acrylic orthosis. C and D: Positioning of the orthosis.
Figure 7 - A: Mold of the orthosis in alginate plate. B: Acrylic orthosis. C and D: Positioning of the orthosis.
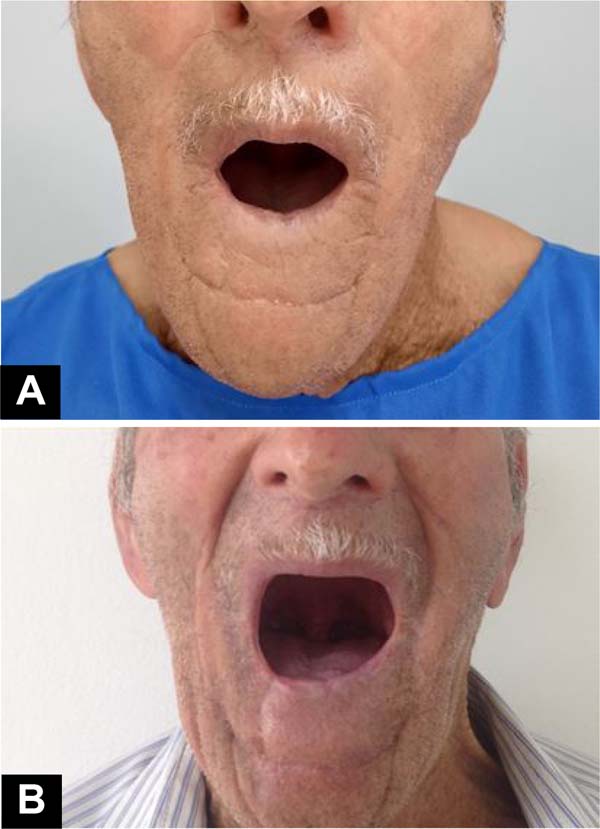
Figure 8 - Postoperative microstomy. A: Before the expansion. B: After expansion.
Figure 8 - Postoperative microstomy. A: Before the expansion. B: After expansion.
The evolution and results were analyzed through regular postoperative follow-up consultations.
RESULTS
Four patients studied, all male, aged between 35 and 77 years, underwent lower lip
reconstruction using the Karapandzic technique, as described in the previous session,
after SCC excision and operated between 2013 and 2022. Three patients who did not
meet the inclusion criteria were excluded from the study.
The most common risk factors for SCC were smoking, alcohol consumption, fair skin,
and chronic sun exposure. The preoperative biopsy (paraffin pathology) confirmed a
diagnosis of well or moderately differentiated SCC, obviously with compromised margins.
Histopathological analysis (in paraffin) of the piece removed after surgery revealed
infiltrating SCC, with depth varying from 3 to 7mm and minimum free surgical margins
of 4mm for all cases (Table 1).
Table 1 - Distribution of the case series according to tumor, surgical, and follow-up aspects.
| Name |
JPPH |
JCQ |
SPF |
MDS |
| Age (years) |
69 |
39 |
77 |
35 |
| Sex |
Masculine |
Masculine |
Masculine |
Masculine |
| Risk factors |
Smoking and alcoholism |
Skin phototype I by Fitzpatrick17 |
Smoking, alcohol consumption, and chronic sun exposure |
Chronic sun exposure and phototype I skin
Fitzpatrick17 |
| Preoperative biopsy (in paraffin) |
Well-differentiated infiltrating SCC |
SCC
moderately differentiated and invasive
|
SCC |
SCC |
| Surgical margins postoperative |
Free |
Free and broad |
Free |
Free |
| Depth |
3mm |
7mm |
6mm |
5mm |
| Postoperative pathology (in paraffin) |
Well-differentiated SCC
and infiltrating
|
Well-differentiated SCC and infiltrating |
Well-differentiated SCC
and infiltrating
|
Well-differentiated SCC
and infiltrating
|
| Postoperative complications |
- |
Hypertrophic scar |
Partial dehiscence and
microstomia
|
Microstomia |
| Follow-up time |
3 months and 6 days |
3 months and 14 days |
7 months and 23 days |
6 months and 18 days |
Table 1 - Distribution of the case series according to tumor, surgical, and follow-up aspects.
No frozen section biopsies were performed in any of these cases.
The complications and complications detected in this study were considered mild. We
found one case of mild hypertrophic scarring and another case of small vermilion dehiscence
of the lip. Microstomia occurred in two of the four operated cases. Severe complications
such as infection, necrosis, and thromboembolic phenomena, among others, did not occur
in this study.
DISCUSSION
In our study series, there were few complications in patients undergoing the Karapandzic
flap, corroborating the idea that this technique meets the needs for lip reconstruction
through large resections, bringing good results, both functional and aesthetic (Figures 9 and 10).
Figure 9 - Pre and postoperative.
Figure 9 - Pre and postoperative.
Figure 10 - Pre and postoperative.
Figure 10 - Pre and postoperative.
Azevedo et al.13 published a case report of two patients who underwent lower lip reconstruction using
the Karapandzic technique. One of the patients presented lip dehiscence at the junction
of the flaps and required a complementary procedure to refine the aesthetic result,
and the other patient had a good aesthetic and functional result without complications.
Matos da Fonseca & Gómez García3 and Guimarães et al.1 published reports on this technique and described the case report of a patient who
underwent reconstruction of the lower lip using the Karapandzic technique with good
evolution, preserving facial mimicry and lip sensitivity, no functional deficit.
Another study, published by Mendes-Abreu et al.16, reported the case of a patient who underwent the Karapandzic flap due to advanced
squamous cell carcinoma of the lower lip, the result of which showed scars filling
the physiological grooves, the maintenance of oral continence, lip sensitivity, and
mobility, although with slight asymmetry and microstomia without functional impact.
The possible intercurrences and/or complications we report follow the available literature.
The published studies do not present a case series with many cases and focus on reporting
the flap creation technique and its complications or postoperative complications.
Although it is important to highlight that most of these authors considered the final
result satisfactory, the most commonly cited complications were lip dehiscence at
the junction of the flaps14, slight asymmetry, and microstomia (reduction of the lip cleft) without functional
impact7.
The flap described by Karapandzic in 1974 is one of the options for the reconstruction
of large lip defects and is based on the anatomical preservation of the facial vascular-nervous
pedicles, which maintains the future irrigation and functionality of the lip, with
the advantage of being done in a single step18,19. We confirmed all these characteristics with our case study and found that this flap
is truly suitable for correcting defects that occupy 40 to 75% of the length of the
lower lip and can be applied inverted to reconstruct the upper lip.
The Karapandzic flap preserves the mobility and sensitivity of the lower lip and oral
continence. Its biggest drawback is microstomia, described by several authors and
which also occurs with other myocutaneous flap techniques, to a greater or lesser
extent, used to reconstruct full-thickness surgical defects13,20.
Regarding microstomia, we observed that there were no reports of serious cases, including
in our study, and we must consider that microstomia is inherent to this technique
and can be described in varying degrees. We chose to improve postoperative results
by complementing the treatment with tissue expansion, seeking to obtain skin of the
same color, texture, and sensitivity without causing damage to the donor area21.
An expansion prosthesis or orthosis to lengthen commissures and fibrotic muscles may
be essential for patients recovering from extensive labral resections. Triad resin
prosthesis and pressure regulating screw have already been described with good results22. The microstomia referred to in the present study (Figure 6) was partially corrected with conservative treatments through dental orthoses specially
made for each case. Devices made of metal and acrylic for temporary, nighttime use
and that promoted tissue expansion of the lower lip.
The advent of controlled expansion had its first clinical use by Neumann23 in 1957 in the reconstruction of the upper pole of the ear and then, in the 1970s,
with Radovan24 in work on breast reconstruction, later supported by Austad & Rose25 in 1982, beginning a new era in reconstructive surgery. Tissue expansion makes it
possible to obtain skin of the same color, texture, and sensitivity without causing
damage to the donor area26.
Another collaboration of this work refers to the use of preoperative color Doppler
ultrasound, which allows flap planning by checking the viability of the vascular pedicle
and the actual positioning of this pedicle, reducing the chances of inadvertent injury
to the vessels during surgery, which could result in total or partial loss of a flap
in a very important area of the face. Furthermore, it is known that smoking is a frequent
risk factor for SCC and has a significant influence on changes in the flow of regional
dermal circulation on the face21.
Therefore, even though it is not absolutely necessary, prior marking of the vascular
pedicle with echoDoppler is a complement that can increase the safety of the flap.
If the unilateral or bilateral viability of the vascular bundle cannot be identified,
as in cases of previous trauma, the possibility of ischemia of this flap must be considered,
and other surgical techniques must be considered.
CONCLUSION
Reconstruction of the lower lip after resection of extensive squamous cell carcinoma
using the Karapandzic technique has proven to be a reliable, safe, and affordable
procedure and can be performed in a single procedure and quickly. Furthermore, the
technique keeps the vascular-nervous pedicle intact, providing good functional and
aesthetic results. Its biggest drawback is the production of microstomia in the early
stages, which gradually improves over time and/or the adoption of special tissue expansion
measures.
1. Hospital São Francisco de Barbacena, Barbacena, MG, Brazil
2. Hospital Universitário Ciências Médicas de Minas Gerais, Belo Horizonte, MG, Brazil
3. Hospital Municipal Odilon Behrens,Belo Horizonte, MG, Brazil
Corresponding author: Marcelo Lima Pupo Nogueira Rua Capitão Aviador Corteleti, 351, Centro, Barbacena, MG, Brazil, Zip Code: 36200-720,
E-mail: marcelolimapn@hotmail.com