INTRODUCTION
Facial paralysis is a condition caused by the involvement of the facial nerve at any
point along its path. Facial movement can be restored using several techniques.
The
masseteric nerve is used as a nerve transfer in facial reanimation surgery to
treat
facial paralysis, with good functional and aesthetic results1, especially when the transfer is
performed to reinnervate the buccal muscles.
Consequently, oral continence and facial expression are permitted, thus improving
the
quality of life of patients. Masseteric nerve transfer can be total or partial,
the
latter as a “babysitting” procedure, with the purpose of maintaining muscle
viability during the axonal regeneration process of transfacial facial nerve
grafts2. The contralateral
facial nerve used as a transfacial graft requires a period of 9 to 12 months for
the
axons to migrate through the graft, causing the facial muscles to be paralyzed
during this time to atrophy. Using the masseteric nerve as a partial nerve transfer
maintains the viability of the transfacial graft.
The innervation of the masseter muscle depends on the mandibular branch of the fifth
cranial nerve (trigeminal nerve). The mandibular nerve leaves the middle cranial
fossa through the foramen ovale to the infratemporal region, where it divides
into
an anterior trunk and a posterior trunk. The temporomandibular nerve originates
from
the anterior trunk, from which the masseteric nerve arises. The masseteric nerve
emerges towards the masseteric region, passing through the mandibular notch, below
the zygomatic arch, reaching the deep surface of the masseter muscle3,4.
The use of the masseteric nerve as nerve transfer produces a minimal masticatory
motor deficit in the masseter muscle since this muscle has proximal branches of
the
descending branch of the masseteric nerve. These allow the masseter muscle to
maintain its masticatory function when the dominant branch is used for nerve
transfer, in the same way as the synergy between the masseter muscle and the
temporal muscle during mastication4.
Therefore, identification of the masseteric nerve is essential for performing this
technique, for which an anatomotopographic study of the approach to this nerve
was
carried out and applied to facial reinnervation surgery.
OBJECTIVE
Study the topographic anatomy of the masseteric nerve approach, specifying the
variations in its relationships with neighboring structures, as well as its path
and
termination, to obtain a rapid approach and dissection of the masseteric nerve.
METHOD
Fifteen masseteric regions were dissected from adult cadavers fixed in formaldehyde.
Dissection material was used to approach the anatomical parts, as well as
photographic equipment, a digital caliper to take measurements, and the use of
Microsoft Windows Excel software for data collection and processing (Figure 1).
Figure 1 - Preauricular approach similar to the facelift approach in the plane
under the superficial musculoaponeurotic system (SMAS).
Figure 1 - Preauricular approach similar to the facelift approach in the plane
under the superficial musculoaponeurotic system (SMAS).
A preauricular approach similar to the in-plane facelift approach under the
superficial musculoaponeurotic system (SMAS) was performed (Figure 2). The incision was made in the skin over the
subzygomatic triangle between the zygomatic arch, the mandibular condyle, and
the
posterior border of the superficial fascicle of the masseter muscle (Figure 3). The masseteric pedicle was dissected
from the inferior border of the zygomatic arch to its entry between the middle
and
deep fascicles of the masseter muscle (Figure 4). The masseteric nerve and masseteric vessels were identified. In addition,
the length of the zygomatic arch was measured and the point of emergence of the
masseter nerve in relation to it was identified, dividing it into three thirds
(anterior, middle, and posterior) (Chart 1).
Chart 1 - Length of the zygomatic arch identifying the point of emergence of the
masseter nerve in relation to it, dividing it into three thirds (anterior,
middle and posterior).
|
Corpse side |
Zygomatic arch length
(mm)
|
Relationship with 1/3 of the zygomatic arch |
Distance from the lower edge of the arcade - point of
emergence at the zygomatic notch (mm)
|
Condyle distance - emergence at the zygomatic
notch
(mm)
|
Length (mm) |
Width at terminal sector (mm) |
Relationship with masseteric A. and V. |
| 1 |
Left |
34.76 |
Posterior |
2.34 |
4.63 |
25.74 |
1.17 |
Superficial |
| 2 |
Left |
39.53 |
Posterior |
10.19 |
11.44 |
20.83 |
1.14 |
Deep |
| 3 |
Left |
44 |
Posterior |
9 |
15.05 |
21.1 |
0.9 |
Deep |
| 4 |
Right |
51.4 |
Posterior |
10.4 |
12.33 |
12.8 |
1.5 |
Superficial |
| 5 |
Right |
41.96 |
Average |
12.41 |
27.91 |
19.7 |
0.58 |
Superficial |
| 6 |
Right |
42.06 |
Anterior |
7.89 |
35.43 |
16.34 |
1.12 |
Deep |
| 7 |
Left |
33.36 |
Posterior |
6.43 |
14.7 |
33.21 |
2.12 |
Deep |
| 8 |
Right |
53.26 |
Average |
16.86 |
21.41 |
21.47 |
3.36 |
Deep |
| 9 |
Left |
25.83 |
Posterior |
8.78 |
16.75 |
13.41 |
1.1 |
Superficial |
| 10 |
Left |
37.34 |
Posterior |
6.1 |
11.94 |
14.04 |
1.75 |
Superficial |
| 11 |
Right |
49.54 |
Posterior |
14.7 |
14.22 |
8.5 |
1.51 |
Superficial |
| 12 |
Right |
28.93 |
Posterior |
11.15 |
8.34 |
11.7 |
1.59 |
Superficial |
| 13 |
Left |
31.55 |
Posterior |
5.31 |
15.64 |
11.52 |
0.9 |
Superficial |
| 14 |
Left |
42.26 |
Posterior |
9.62 |
5.11 |
23.31 |
2.38 |
Deep |
| 15 |
Right |
50.45 |
Posterior |
1.9 |
5.4 |
18.6 |
1.9 |
Deep |
Chart 1 - Length of the zygomatic arch identifying the point of emergence of the
masseter nerve in relation to it, dividing it into three thirds (anterior,
middle and posterior).
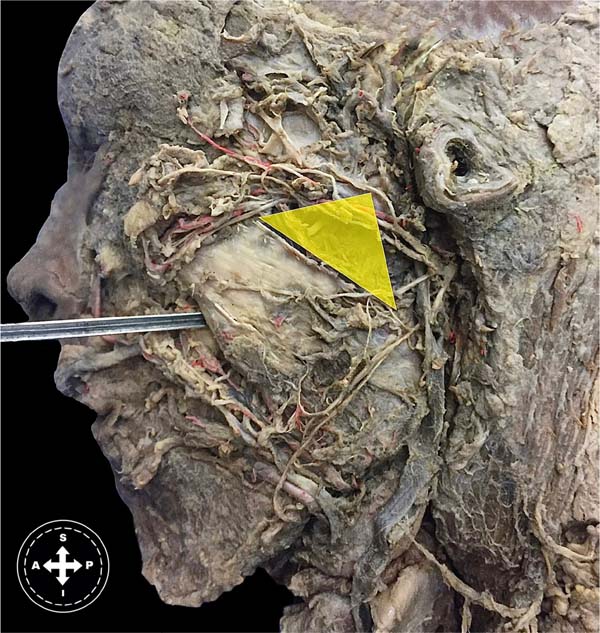
Figure 2 - The subzygomatic triangle between the zygomatic arch, the mandibular
condyle, and the posterior border of the superficial fascicle of the
masseter muscle.
Figure 2 - The subzygomatic triangle between the zygomatic arch, the mandibular
condyle, and the posterior border of the superficial fascicle of the
masseter muscle.
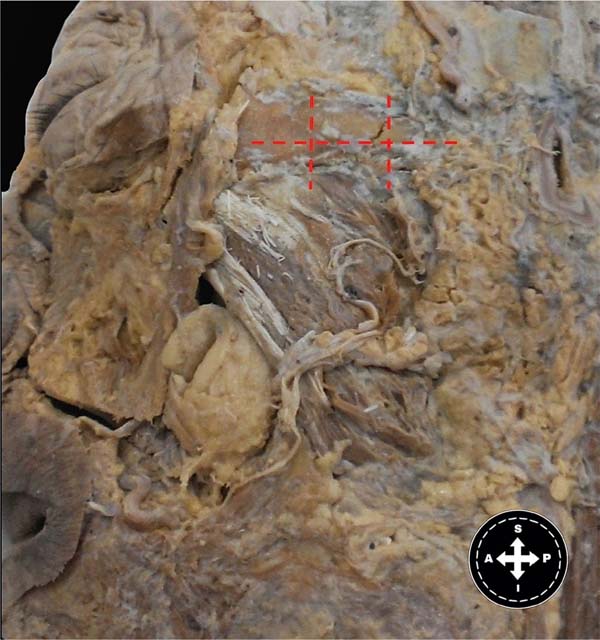
Figure 3 - Masseteric pedicle dissected from the lower edge of the zygomatic
arch to its entry between the middle and deep fascicles of the masseter
muscle.
Figure 3 - Masseteric pedicle dissected from the lower edge of the zygomatic
arch to its entry between the middle and deep fascicles of the masseter
muscle.
Figure 4 - Emergence of the masseter nerve in relation to it, dividing it into
three thirds (anterior, middle, and posterior).
Figure 4 - Emergence of the masseter nerve in relation to it, dividing it into
three thirds (anterior, middle, and posterior).
The relationship between the masseteric nerve and the masseteric vessels was also
verified. The distance of the masseteric nerve course was measured from its
emergence under the zygomatic arch to its termination. Then, the distance between
the mandibular condyle and the point of emergence of the masseteric nerve under
the
zygomatic arch was measured. Finally, the distance between the origin of the
masseteric nerve and the lower border of the zygomatic arch was measured (Figure 4).
RESULTS
The length of the zygomatic arch varied between 53.3 mm and 25.8 mm, with an average
length of 40.4 mm and a median of 42.0 mm.
The emergence of the masseteric nerve was below the posterior third of the zygomatic
arch in 80% of cases, below the middle third in 13%, and below the anterior third
in
7%.
The distance between the inferior border of the zygomatic arch and the emergence of
the masseteric nerve below it ranged from 16.9 mm to 1.9 mm, with a mean of 8.9
mm
and a median of 9.0 mm. The distance between the mandibular condyle and the
emergence point of the masseteric nerve below the zygomatic arch ranged from 35.4
mm
to 4.6 mm, with a mean of 14.7 mm and a median of 14.2 mm.
In 53% of cases, the masseteric nerve was found superficial to the masseteric
vessels, while in 47%, it was found deep to the masseteric vessels.
The length of the masseteric nerve path from its origin under the zygomatic arch to
its termination varied from 33.2 mm to 8.5 mm, with an average of 18.2 mm and
a
median of 18.6 mm.
The width of the nerve at its termination varied from 3.4 mm to 0.6 mm, with an
average of 1.5 mm and a median of 1.5 mm.
DISCUSSION
To topography the masseteric nerve, two palpable anatomical references on the surface
were used: the mandibular condyle and the lower border of the zygomatic arch.
These
present little variability, and their anatomy is not distorted during the surgical
procedure. Collar et al.1 propose
the subzygomatic triangle for the topography of the masseteric nerve. This triangle
is delimited by the zygomatic arch, a vertical line that passes through the
mandibular condyle and the frontal branch of the facial nerve and is a questionable
region for dissection of the masseteric nerve due to the presence of a structure
with variable anatomy such as the frontal branch of the facial nerve.
Using the mandibular condyle, the lower border of the zygomatic arch, and the
posterior border of the masseter muscle, a triangle with more precise limits can
be
determined to topograph the masseteric nerve, reinforcing a more accurate tool
for
facial reanimation surgery with nerve transfer of said nerve.
CONCLUSION
Reliable anatomical relationships have been determined for the identification of the
masseteric nerve during masseteric-facial transfer surgery. It can be identified
in
an area between the zygomatic arch, masseter muscle, and mandibular condyle.
REFERENCES
1. Collar RM, Bryne PJ, Boahene KDO. The subzygomatic triangle: rapid,
minimally invasive identification of the masseteric nerve for facial
reanimation. Plast Reconstr Surg. 2013 Jul;132(1):183-8. DOI:
10.1097/PRS.0b013e318290f6dc
2. Rodriguez ED, Neligan PC. Plastic surgery: Volume 3: Craniofacial,
head and neck surgery and pediatric plastic surgery. 4th ed.
Philadelphia; Elsevier; 2017.
3. Kaya B, Apayadin N, Loukas M, Tubbs RS. The topographic anatomy of
the masseteric nerve: A cadaveric study with an emphasis on the effective zone
of botulinum toxin A injections in masseter. J Plast Reconstr Aesthet Surg.
2014;67(12):1663-8. DOI: 10.1016/j.bjps.2014.07.043
4. Cotrufo S, Hart A, Payne AP, Sjogren A, Lorenzo A, Morley S.
Topographic anatomy of the nerve to masseter: an anatomical and clinical study.
J Plast Reconstr Aesthet Surg. 2011;64(11):1424-9. DOI:
10.1016/j.bjps.2011.05.026
1. Facultad de Medicina Universidad de la
Republica, Departamento de Anatomía, Montevideo, Montevideo,
Uruguai
2. Facultad de Medicina Universidad de la
República, Cátedra de Cirugía Plástica Reparadora y Estética Hospital de
Clínicas, Montevideo, Montevideo, Uruguai
Joaquín Calisto Tacuarembó
1429/315, Montevideu, Uruguai, E-mail: joaquin.calisto@gmail.com
Artigo submetido: 06/08/2023.
Artigo aceito: 26/07/2024.
Conflicts of interest: none.