

Review Article - Year 2024 - Volume 39 -
Effect of using taping in the postoperative period of plastic surgery: A systematic review
Efeito do uso do taping no pós-operatório de cirurgias plásticas: Uma revisão sistemática
ABSTRACT
Pain is the main complaint after plastic surgery. Despite existing medications, musculoskeletal discomfort, edema, and bruising greatly affect a woman's quality of life. Physiotherapy has some techniques to minimize these effects, and taping has been widely used in clinical practice, but without robust scientific evidence. Thus, the objective of the present work was to systematically review published studies on taping in the postoperative period of plastic surgery. Electronic searches were carried out without restrictions on language or year of publication in the MEDLINE databases via PubMed, Embase, CINAHL, LILACS, PEDro, and SPORTDiscus on March 20, 2023. The keywords "cirurgia plástica" and "taping" were used. Clinical trials and case studies were included in the postoperative period with pain symptoms and taping as an intervention method. Data extraction was carried out by two independent evaluators, using the Endnote X8 software. A total of 590 articles were found in the databases, of which 47 were considered eligible for full reading and 6 were included for analysis. Among the results achieved with the use of this resource, reduction in edema, pain, bruising, and shorter post-surgical recovery time were mentioned. Therefore, through this review, it was possible to verify that taping has a beneficial effect on pain compared to no treatment. However, the low methodological quality of the studies and sample limitations are limiting factors. Therefore, it is recommended that more research should be carried out, with controlled and randomized clinical trials, so that there are strong and consistent results.
Keywords: Plastic surgery procedures; Pain; Edema; Fibrosis; Athletic tape.
RESUMO
A dor é principal queixa no pós-operatório de cirurgia plástica. Apesar das medicações existentes, o desconforto musculoesquelético, edema e equimoses afetam muito a qualidade de vida da mulher. A fisioterapia possui algumas técnicas para minimizar esses efeitos, e o taping tem sido amplamente utilizado na prática clínica, porém sem evidência científica robusta. Assim, o objetivo do presente trabalho foi revisar sistematicamente estudos publicados sobre taping no pós-operatório de cirurgias plásticas. As buscas eletrônicas foram realizadas sem restrição de linguagem ou ano de publicação nas bases de dados MEDLINE via PubMed, Embase, CINAHL, LILACS, PEDro, e SPORTDiscus em 20 março de 2023. Foram utilizadas as palavras-chave "cirurgia plástica" e "taping". Ensaios clínicos e estudos de caso foram incluídos no período pós-operatório com sintomas álgicos e taping como método de intervenção. A extração dos dados foi feita por dois avaliadores independentes, utilizando o software Endnote X8. Um total de 590 artigos foi encontrado nas bases de dados, destes, 47 foram considerados elegíveis para leitura completa e 6 foram incluídos para análise. Dentre os resultados alcançados com a utilização deste recurso, foram citados redução de edema, dor, equimose, e menor tempo de recuperação pós-cirúrgico. Portanto, por meio desta revisão, foi possível verificar que o taping promove um efeito benéfico sobre a dor em comparação com nenhum tratamento. Entretanto, a baixa qualidade metodológica dos estudos e a limitação amostral são fatores limitantes. Assim, recomenda-se que mais pesquisas devem ser realizadas, com ensaios clínicos controlados e randomizados, para que haja resultados fortes e consistentes.
Palavras-chave: Procedimentos de cirurgia plástica; Dor; Edema; Fibrose; Fita atlética.
INTRODUCTION
Dermatofunctional physiotherapy is a physiotherapy specialty recognized by Resolution No. 362/2009, which studies and acts on the integumentary system and structures related to human functionality in the entire clinical-kinesiological-functional expression of individuals with changes in skin functions.
The role of dermatofunctional physiotherapy in the pre- and post-operative period of plastic surgery is to promote and restore the individual’s health and quality of life. Through the use of resources that enhance the physiological mechanisms of tissue repair and blood and lymphatic microcirculation, pain and discomfort relief is achieved, thus helping to improve the patient’s functionality and also preventing possible complications of the surgical procedure and the period of immobilization to which it is exposed1.
Pain is one of the most common complaints at this time, and it will occur proportionally in response to the inflammatory process of the interventions carried out during surgery. Therefore, opting for interventions that can control this initial response will ensure greater patient comfort and may contribute to maintaining functionality and recovery time2, 3.
Another consequence of surgical procedures is ecchymosis, which is generated due to the mechanical trauma of the surgical intervention and causes rupture of subcutaneous microvessels. This leads to intravascular leakage into adjacent soft tissues, such as the skin, causing reddish and purple spots. Early intervention in these cases prevents the formation of spots and possible local fibrosis. In more serious cases of rupture of larger vascular structures, hematomas occur, which are controlled with intervention by the responsible surgeons.
Furthermore, edema also occurs due to trauma caused to the tissue, forming an inflammatory process that follows the swelling4. This accumulation of edema directly interferes with the quality of the individual’s range of motion, as well as their pain condition, and it is also extremely important to adopt strategies to improve this symptom5.
The entry of Dermatofunctional Physiotherapy into the surgical environment has gained prominence in recent times. Pre- and post-operative interventions have been considered important in this scenario for optimizing the symptoms mentioned above.
Among the alternatives that can be used, intending to accelerate the patient’s rehabilitation, one that has received a lot of attention is the application of taping immediately after the completion of the surgical intervention6. The possible physiological effects of taping are due to the elastic nature and the way it is applied. It can be indicated for the control of pain caused by sensory impact on mechanoreceptors by pressure, tension, elevation, compression, and traction of the skin7 or by the stimulation of large diameter fibers, according to Melzac and Wall’s theory8 of the “closing of the floodgates” in posterior column of the spinal cord, resulting in the release of endogenous opioids at the brain and spinal cord9.
Furthermore, due to the difference in pressure gradient generated by applications in the form of tails and the stimulation at the level of the dermis and epidermis through convolutions that generate cavities, therefore, they act to significantly improve the circulation of fluids, blood and lymph stagnant in local inflammatory processes7.
Studies that use taping to control the symptoms mentioned above, resulting from plastic surgery procedures, are currently scarce. This raises some concern, given that the use of this resource is on the rise, even without scientific support. The clinical reasoning for its use has therefore been based on studies carried out in the use of orthopedic conditions.
A systematic review of the clinical effect of taping included eight randomized and controlled clinical trials, six with patients with musculoskeletal disorders, one with post-breast cancer lymphedema, and another with post-stroke patients. Six of these studies included a placebo-taping group10. It was concluded that given the high use of this resource clinically in the current scenario, its evidence is moderately limited, however, analyzing the results of the applications, taping is more clinically effective than placebo. Thus, the combination of taping with the conventional physiotherapeutic approach is effective for pain control10.
A second systematic review evaluated the effect of taping on chronic low back pain and included five studies, involving 306 subjects, concluding that taping should not be used as a substitute for conventional physiotherapy or physical exercise, with taping being more effective when used as an adjunct to therapy, promoting improvement in range of motion and pain11.
Another more recent systematic review on the effect of taping on pain resulting from patellofemoral syndrome evaluated five randomized and controlled clinical trials with 235 patients and concluded that taping for pain in this syndrome should only be used as a complementary therapeutic resource to traditional exercise therapy and not support for using the taping in isolation12. Finally, a recent systematic review evaluated the effect of taping on low back pain in pregnant women and analyzed seven studies with 444 patients, concluding that taping has a positive effect on improving low back pain during pregnancy with positive impacts on the quality of life of these women13.
OBJECTIVE
In this context, it is observed that the use of taping has been increasingly used in clinical practice, however, without scientific evidence in the dermatofunctional area that proves its effectiveness in the post-surgical rehabilitation process. Therefore, the objective of the present work was to systematically review published studies on taping in the postoperative period of plastic surgery.
METHOD
Inclusion criteria for studies in this review
Types of studies
This systematic review had its protocol registered in PROSPERO (International Prospective Registry of Systematic Reviews) under number CD42022339803. Clinical trials and case studies published from 2013 to March 2023, in the postoperative period of plastic surgeries, which investigated the effects of taping on pain as a primary outcome, and edema, ecchymosis, fibrosis, and adverse effects as secondary outcomes were included. Observational studies, systematic reviews, and other types of physical exercise treatments were excluded.
Types of interventions
Clinical trials were analyzed that compared taping in the immediate post-surgical period with the control group that underwent conventional medical monitoring or conventional physiotherapy and that evaluated non-specific pain. Studies including chronic pain were not included.
Types of results
The primary results were considered: Reduction in pain, assessed using a specific instrument for assessing the level of pain or other general assessment instruments, as long as they can adequately assess the level of non-specific pain. Furthermore, secondary results were edema, bruising, fibrosis, adverse effects, and safety of using the technique.
Search methods for identifying studies/Electronic searches
The studies selected in this review were found through an electronic search in the following databases: Literature Database and Retrieval System Online (MEDLINE), Excerpta Medical Database (EMBASE), Latin American and Caribbean Health Sciences (LILACS), Cumulative Index to Nursing and Allied Health Literature (CINHAL), Physiotherapy Evidence Database (PEDro), SPORTDiscus and Cochrane Library for relevant articles published from 2013 to March 2023.
The searches were carried out individually for each database. The search strategy adopted for MEDLINE via PubMed was: “plastic surgery procedures” OR “surgery, plastic” AND “Tape, Atletic” OR “Orthotic Tape” OR “Tape, Orthotic” OR “Kinesio Tape” OR Kinesio Tapes” OR “ Tape, Kinesio” OR “Tapes, Kinesio” OR “Kinesiotape” OR “Bandages”. Filters for the type of studies, publication time, or language were not applied. This strategy was adapted to other databases.
Data collection and analysis
Study selection, data extraction, and management
The selection of studies was carried out by two independent evaluators, using the Endnote X8 software, initially analyzing the title and summary of the references found through the database search strategy. Studies considered potentially eligible were evaluated, and disagreements were discussed among the reviewers in search of consensus before the final inclusion of the studies.
Data extraction was carried out using a form previously prepared and tested by the authors. Studies referenced in more than one publication, when eligible, had their data computed only once. The following study characteristics were extracted: methods, participants, interventions, results, and statements of interest. The selection process was documented with a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart.
Treatment outcomes and effects
For primary and secondary outcomes for which there were sufficient data, we conducted a meta-analysis using fixed or randomized effects models according to the specificity of available data.
The overall quality of the body of evidence for the primary outcome of this review (musculoskeletal pain) was assessed using the GRADE criteria (study limitations, consistency of effect, imprecision, indirectness, and publication bias).
RESULTS
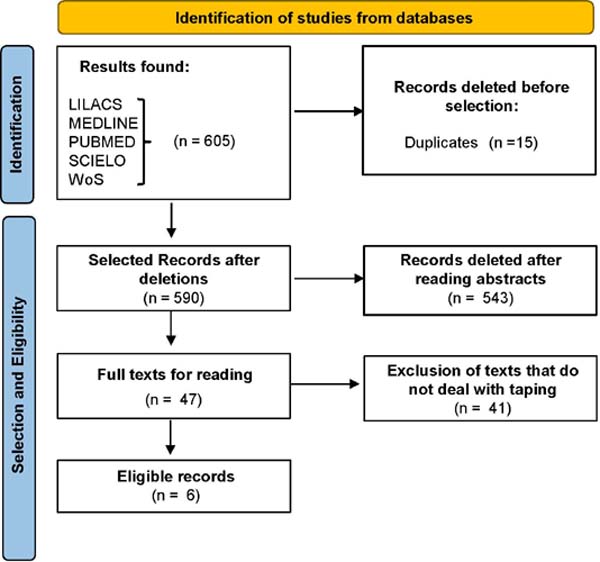
Through an electronic search, 605 records were found in the chosen databases, of which 15 were excluded due to duplication. The remaining 590 were selected through title and abstract reading and 549 articles were excluded for not meeting the inclusion criteria.
A total of 47 records were selected for analysis through full reading, 41 were excluded for not meeting the criteria and 6 were considered eligible for this review and included in the qualitative and quantitative analysis according to the PRISMA flowchart (Figure 1). After reading the articles in full, they were organized with the following information (Table 1): type of study, characteristic of the intervention, objective, variables analyzed, evaluation instrument, and results achieved.
| Publication | Type of Study | Characteristics of the Intervention | Objective | Variables Analyzed | Assessment Instrument | Results |
|---|---|---|---|---|---|---|
| (Paula, 2017). | Case study | N: 1, sex F, 25 years old. Use of manual techniques release associated with taping application about fibrosis and adhesions reapplied to every 7 days for 5 sessions | Describe the taping effects in treatment of fibrosis and adhesions scars on postoperative liposuction | Fibrosis | Palpation and pho-todocumentation | The presence of fibrosis was observed only through palpation. THE patient also reported improvement tissue mobility and appearance visual at the end of treatment |
| (Chi et al., 2016) | Clinical trial no randomized. Groups: Phase remodeling; Phase proliferation | N: 10, gender F, Age: 44 to 51 years old Method: 10 sessions, 2x/week. With intervals of 2 or 3 days. Remodeling phase - DLM and taping, associated with therapy combined (US + current excitomotor) Phase proliferation - DLM and taping | Identify the effects of two protocols different in the treatment of fibrosis secondary to postoperative of abdominoplasty and liposuction of abdomen | Fibrosis | Palpation; Thermography of contact | The comparative analysis of the evaluation initial and final, both from palpation as for thermography, it showed that there was a significant reduction (p< 0.0001) of the fibrotic condition presented by patients. |
| (Chi et al., 2021) | Controlled clinical trials and non-randomized Group: GE – Treat. Intra-op GC | N: 20 Age: 20 to 60 years Method: GE (10) - Taping Intraop. Intraop treatment and reevaluated on the 4th day post-op. GC (10) - without intervention | Evaluate the occurrence of bruising in patients undergoing AP associated with traditional ABD LA | Pain and bruise | Documentation EVA photographic | GE presented a better response in resolving bruising (p = 0.01) compared to the control group |
| (Chi et al., 2018) | Controlled clinical study. (n=20) | N: 20, sex F. Age: 18 and 56 years old. Total of 15 sessions. GE: pre, trans, and post-op care. GC: service on the 4th day. The resources used were DLM, microcurrents, red LED, and taping in the operated area | Propose an unprecedented approach from the pre-, trans- and post-operative stages to prevent and minimize fibrosis, edema, and ecchymosis | Ecchymosis, edema, and fibrosis | Palpation, contact thermography; photodocumentation, perimetry |
The occurrence of fibrosis in the EG was statistically (p = 0.003) lower than in the CG; lower degree of fibrosis in EG (p=0.0002); and the initial thermography was predominantly normal in the EG (p=0.0002); no occurrence of intense edema in the EG (0.035); non-occurrence of bruising was greater in EG (p=0.0056) |
| (Pelissaro, 2022) | Experimental thesis | N: 28 Age: 18 to 19 years old. After bichectomy. Group I: Control Side: Without intervention. Treated Side: 2 taping strips in the region external jugal of the face by 2 days, intraoperatively. Group II: Hemiface- laser low power 6J/cm2, intraoperative and day 2. Control Side: Without intervention | Assess the effect taping and low laser power in post-op bichectomy | Facial anthropometry and Edema | Tape measure millimeter, for edema, they were carried out three times, being the first immediately before the procedure surgical and too much after 2 and 7 days. Ultrasound for pre, post immediate and after 6 months | The results showed a reduction significant edema after taping for 2 days post-surgery (p<0.001), something that was not observed with laser therapy (p=0.127) |
| (Moraes, 2012). | Case study | N:l, female, 60 years old. 10 sessions, twice a week, application of DLM and taping, in each session | Check the results before the application of DLM and taping, in pain, edema, bruise and pigmentation of abdomen and breasts on rehabilitation after liposuction to reconstruction mammary | Pain, edema, hematoma and pigmentation | Classification of intensity of pain: EVN and soft tissues: perimetry thoracic and abdominal and recording photographic | Pain intensity was classified as 4 in the 1st assessment, with ↓, to 2 in the 2nd evaluation and to 0 in the EVN from the 3rd session. The perimeter ↓, in all places of measurement from the 1st assessment to the 6th session. The scars presented changes, as that on both breasts increased their mobility tissue and reduced adhesions |
Included studies and participants
Six (n=6) studies were included in the literature review, all studies being conducted in Brazil. Two studies are case studies, and four are controlled clinical trials.
In the analysis of the six studies, 41 participants were included in this review, all adult women (18 to 60 years old) in the postoperative period of plastic surgery. One study included women in the post-bichectomy period, four studies included post-liposuction women, and two studies included post-abdominoplasty women. The average age of the studied population was 39 years, with 18 being the youngest14 and 60 being the oldest15.
Interventions
The three clinical trials compared taping with conventional and multimodal physiotherapeutic treatment including cryotherapy, lymphatic drainage, and microcurrents. In the study by Chi et al.15, the taping group was compared with a control group without intervention, with only medical monitoring. In the study by Pelissaro14, the control group received only cryotherapy.
Type of application, frequency, duration, and treatment time
In the study by Pelissaro14, the taping was applied to the face, in a “Y” shape, with minimal tension for 2 days. In the study by Chi et al.15, three types of “web” or “basket” cuts were used for fibrosis, “fan” or “octopus” cuts for edema, and “hashtag” cuts for bruises, kept for 3 to 5 days. with skin rest for 1 day before the next application.
In the study by Chi et al.16, taping was applied in a Fan or “octopus” format for a period of 3 days. Finally, in the Morais17 study, taping was applied to the abdomen and breast regions in the shape of an “octopus”, twice a week.
Outcomes and effects of treatment
Primary outcomes
Two studies reported musculoskeletal pain symptoms as outcomes and were included. The same assessment instruments were used to measure pain intensity using the visual analog scale (VAS). The study by Morais17 also evaluated pain. A summary of information about the studies included in this review is presented in Table 1.
Secondary outcomes
Three articles (Pelissaro14, Morais17, and Chi et al.4) evaluated the outcome of edema using perimetry. Pelissaro14 evaluated facial edema after bichectomy surgery. Morais17 and Chi et al.4 evaluated edema after abdominoplasty and liposuction surgery. A single study, by Chi et al.16, evaluated the outcome of fibrosis through palpation and visual inspection applied to a scale and also thermography. None of the studies evaluated the safety and adverse effects of the taping technique after plastic surgery.
Allocation
Of the clinical trials included in the study, none of them report how the allocation and blinding of participants were carried out, and it is understood that it occurred for convenience, which means that there was an allocation bias.
Blinding participants and professionals
None of the included studies described blinding methods and all were categorized as having a high risk of bias and were therefore categorized as having a clear risk of bias.
Incomplete results
None of the included studies reported significant losses related to treatment, being categorized as a moderate risk of bias.
DISCUSSION
The surgical procedure will cause initial trauma to the target tissue, this trauma will generate an inflammatory process which, in turn, will promote scar tissue for the recovery of this area, that is, tissue not identical to the initial tissue. This will happen at the edges of the scar and also in the subcutaneous region, where all the tissue will be detached, known as “dead space”18.
Following resolution No. 394/2011 of the Federal Council of Physiotherapy and Occupational Therapy (COFFITO), the physiotherapist is the professional with the aptitude to conduct the post-operative period and promote the complete rehabilitation of the patient, leading the healing process, minimizing intercurrences, complications and favoring the final result of the surgery. This professional is recommended by the Sociedade Brasileira de Cirurgia Plástica to conduct post-operative care, due to the training of this professional, which goes far beyond carrying out treatment that aims only at aesthetic results1.
Soon after the end of the surgery, the inflammatory phase begins. Edema is very characteristic during this period and occurs due to the imbalance of interstitial fluid reabsorption due to the loss of integrity of local blood and lymphatic flow19.
This phase of imbalance in this function causes pain and discomfort, and has a high incidence, making it necessary for the patient to use medication to alleviate it. However, every medication has side effects, so it must be used rationally and as prescribed by the doctor. To provide efficient and resolute care, physiotherapy can be a good ally for improving pain through the use of therapeutic resources. Among the range of resources available, taping has currently been widely used in this scenario1.
Its use aims to reduce pain and reduce edema and ecchymosis in the post-operative period of plastic surgery, all depending on the tension applied and the way the tape is cut, which will promote physiological effects through the principle of response to tensegrity and cellular mechanotransduction, which is the ability to translate a mechanical stimulus into cellular activity. This happens due to the conversion of information during the interaction of the extracellular matrix with local mechanoreceptor cells20.
It is believed through clinical and scientific evidence that the use of intact taping with high tensions has good results for containing inflammation and initial edema, by reducing the space between the tissues below1. As for using the tape with light tension, its principle is that it can promote decompression of the tissue below, promoting greater fluidity in lymphatic and blood irrigation. Among these applications, the “web” or “basket” cut has good results for fibrosis, the “fan” or “octopus” cut has good results for edema, and the “hashtag” cut has good results for bruises15, 16.
The results achieved have been a great ally applied in current clinical practice, and the results found in this review corroborate this statement. However, there are still few studies that evaluate its scientific evidence in the postoperative period of plastic surgery in particular.
This is the first systematic review to investigate the effectiveness of taping in this scenario and we found that there are still few studies of high methodological quality and representative samples on the effectiveness of taping in the treatment of non-specific pain, for this reason, the results should be analyzed with caution.
In our systematic review, we only included studies published as full articles in journals indexed in databases that undergo rigorous peer review, which is actually carried out by an expert in the field. Studies that have not been subjected to peer review may have a greater risk of bias or negative results, and their inclusion in systematic reviews is not recommended.
The results obtained in this review are related to the effects analyzed after the short-term intervention (immediately after the intervention), as there are not yet enough studies for meta-analysis in comparing the effects of taping over time. To this end, more studies that evaluate the effectiveness of this method for this population must be carried out.
Furthermore, there are no studies that support standardization of treatment duration, weekly frequency, intensity, and types of taping cuts appropriate for patients with non-specific pain. The studies analyzed were similar concerning the control group, in which the patients were under medical and nursing care in a conventional pre-surgical setting.
Another issue to be raised is the lack of standardization of the nomenclature used to refer to the technique. Among the articles analyzed, we found neuromuscular taping, linfotaping, taping, kinesiotherapy, and Punch Tape. This variety of nomenclature hinders the search for data regarding the effectiveness of the technique.
CONCLUSION
Taping was associated with a beneficial effect on pain compared with no treatment. However, the low methodological quality of the studies and sample limitations are limiting factors. There is no evidence to support the use of taping to replace other conventional physiotherapy modalities, and this resource should be used in a complementary way to dermatofunctional physiotherapy (exercise and manual therapy) in the postoperative period of plastic surgery.
REFERENCES
1. Pegorare ABS, Oliveira Júnior SA, Tibola J. Manual de condutas e práticas em fisioterapia dermatofuncional: atuação no pré e pós operatório de cirurgias plásticas. Campo Grande: UFMS; 2021.
2. Oliveira CMB, Issy AM, Sakata RK. Fisiopatologia da dor pós-operatória. Rev Bras Med. 2010;67(11):415-8.
3. Schoenbrunner AR, Janis JE. Pain Management in Plastic Surgery. Clin Plast Surg. 2020;47(2):191-201.
4. Chi A, Lange A, Guimarães MVTN, Santos CB. Prevenção e tratamento de equimose, edema e fibrose no pré, trans e pós-operatório de cirurgias plásticas. Rev Bras Cir Plást. 2018;33(3):343-54.
5. Petrova TV Koh GY. Biological functions of lymphatic vessels. Science. 2020;369(6500):eaax4063.
6. Correa LN, Sousa EB, Oliveira NPC. O uso do taping no pós-operatório de cirurgia plástica. Res Soc Dev. 2021;10(15):e81101522868.
7. Wu WT, Hong CZ, Chou LW The Kinesio Taping Method for Myofascial Pain Control. Evid Based Complement Alternat Med. 2015;2015:950519.
8. Rachlin H. Dor e comportamento. Temas Psicol. 2010;18(2):429-47.
9. Gosling AP. Mecanismos de ação e efeitos da fisioterapia no tratamento da dor. Rev Dor. 2012;13(1):65-70.
10. Morris D, Jones D, Ryan H, Ryan CG. The clinical effects of Kinesio® Tex taping: A systematic review. Physiother Theory Pract. 2013;29(4):259-70.
11. Nelson NL. Kinesio taping for chronic low back pain: A systematic review. J Bodyw Mov Ther. 2016;20(3):672-81.
12. Logan CA, Bhashyam AR, Tisosky AJ, Haber DB, Jorgensen A, Roy A, et al. Systematic Review of the Effect of Taping Techniques on Patellofemoral Pain Syndrome. Sports Health. 2017;9(5):456-61.
13. Xue X, Chen Y, Mao X, Tu H, Yang X, Deng Z, et al. Effect of kinesio taping on low back pain during pregnancy: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2021;21(1):712.
14. Pelissaro GS. Efeito da kinesioterapia e do laser de baixa potência no pós-operatório de bichectomia, em pacientes com trauma mastigatório recorrente [Tese de doutorado]. Campo Grande: Universidade Federal de Mato Grosso do Sul; 2022.
15. Chi A, Marquetti MG, Dias M. Uso do taping linfático na prevenção da formação de equimoses em abdominoplastia e lipoaspiração. Rev Bras Cir Plást. 2021;36(2):144-50.
16. Chi A, Oliveira AVM, Ruh AC, Schleder JC. O uso do linfotaping, terapia combinada e drenagem linfática manual sobre a fibrose no pós-operatório de cirurgia plástica de abdome. Fisioter Bras. 2016;17(3):197-203.
17. Morais SC. O efeito da drenagem linfática manual e das bandas neuromusculares na reabilitação pós-lipoaspiração para reconstrução mamária: estudo de caso [Trabalho de conclusão de curso]. Porto: Universidade Fernando Pessoa; 2012.
18. Li J, Jung W, Nam S, Chaudhuri O, Kim T. Roles of Interactions Between Cells and Extracellular Matrices for Cell Migration and Matrix Remodeling. In: Zhang Y, ed. Multi-scale Extracellular Matrix Mechanics and Mechanobiology. Cham: Springer; 2020. p. 247-82.
19. Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound healing: a cellular perspective. Physiol Rev. 2019;99(1):665-706.
20. Fu S, Panayi A, Fan J, Mayer HF, Daya M, Khouri RK, et al. Mechanotransduction in Wound Healing: From the Cellular and Molecular Level to the Clinic. Adv Skin Wound Care. 2021;34(2):67-74.
1. Universidade Federal de Mato Grosso do Sul, Instituto Integrado de Saúde, Campo
Grande, MS, Brazil
Corresponding author: Ana Beatriz Gomes de Souza Pegorare Cidade Universitária, s/n Universitário-900, Campo Grande, MS, Brazil. Zip Code: 79070-900. E-mail: ana.pegorare@ufms.br





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter