

Case Report - Year 2020 - Volume 35 -
Management of constricted ear: plastic surgery service approach at the Hospital of Clinics in Porto Alegre, Brazil
Manejo da orelha constricta: abordagem do serviço de cirurgia plástica do Hospital de Clínicas de Porto Alegre, Brasil
ABSTRACT
Introduction: The prevalence of ear malformations reaches
5% when considering the entire world population. Primarily
presented in 1975, the constricted ear represents a group of
deformities of the upper third of the auricular cartilage with
common features. The aesthetic impact and social stigma
of these deformities can cause psychological harm to the
patient when not corrected.
Methods: We describe below
the technique used in the plastic surgery department of the
Hospital de Clínicas de Porto Alegre.
Results: Result can
be evidenced with 30 days postoperatively.
Conclusion: The
described method, cartilage resettlement, is an option for
treatment of this deformity with adequate aesthetic result.
Keywords: Multiple trauma; Wounds and injuries; Plastic surgery; Wound closure techniques; Autologous transplantation.
RESUMO
Introdução: A prevalência de malformações da orelha chega a 5% quando considerada toda a população mundial. Primariamente descrita em 1975 a orelha constricta representa um grupo de deformidades envolvendo o terço superior da cartilagem auricular com características em comum. O impacto estético e o estigma social dessas deformidades podem levar a danos psicológicos ao paciente quando não corrigidos.
Métodos: Descrevemos a seguir a técnica utilizada no serviço de cirurgia plástica do Hospital de Clínicas de Porto Alegre.
Resultados: O resultado pode ser evidenciado com 30 dias de pós-operatório.
Conclusão: O método descrito, de reacomodação da cartilagem, é uma opção para o tratamento dessa deformidade com adequado resultado estético.
Palavras-chave: Deformidades adquiridas da orelha; Orelha; Cartilagem da orelha; Orelha externa; Otopatias
INTRODUCTION
The prevalence of ear malformations reaches 5% when considering the entire world population1. Primarily described in 1975, the constricted ear represents a group of deformities involving the upper third of the auricular cartilage with four characteristics in common: 1. Edge of the helix excessively curved due to disappearance or decrease of the scapha, triangular fossa, and upper cross; 2. Protrusion, caused by the flattening of the anti-helix and the helix’s edge, resulting in a deep concha; 3. Low implantation of the ear; 4. Global decrease in ear size2.
These deformities’ aesthetic impact and social stigma can lead to psychological damage to the patient when not corrected. The constricted ear is classified as mild, moderate, and severe according to the degree of impairment and deformity of the auricular cartilage, influencing the choice of method and the ideal time for treatment.
Mild deformities eventually resolve spontaneously or with non-surgical management through ear molds and immobilization; however, moderate to severe degrees are invariably treated with surgical management, as shown below3.
CASE REPORT
We describe the plastic surgery service approach at the Hospital de Clínicas de Porto Alegre with the modification of the cartilaginous flap technique described by Tanzer, in 19752, for the treatment of constricted ears deformity. This technique is used routinely in the service for treating constricted ear.
The patient involved signed an informed consent form. The research followed the Helsinki principles.
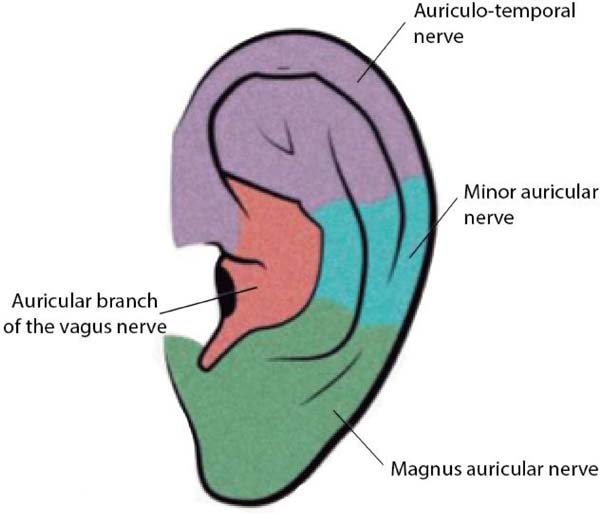
Anesthetic block with 2% lidocaine and 7.5% ropivacaine with vasoconstrictor at a concentration of 1: 100,000 in the region of innervation of the auricular branch of the vagus nerve (tragus), auricular magnum (lobe), minor occipital (middle third of the helix) and auriculotemporal (helix and tragus) (Figure 1).
Hydrodissection of the cutaneous layer in the anterior and posterior region of the concha.
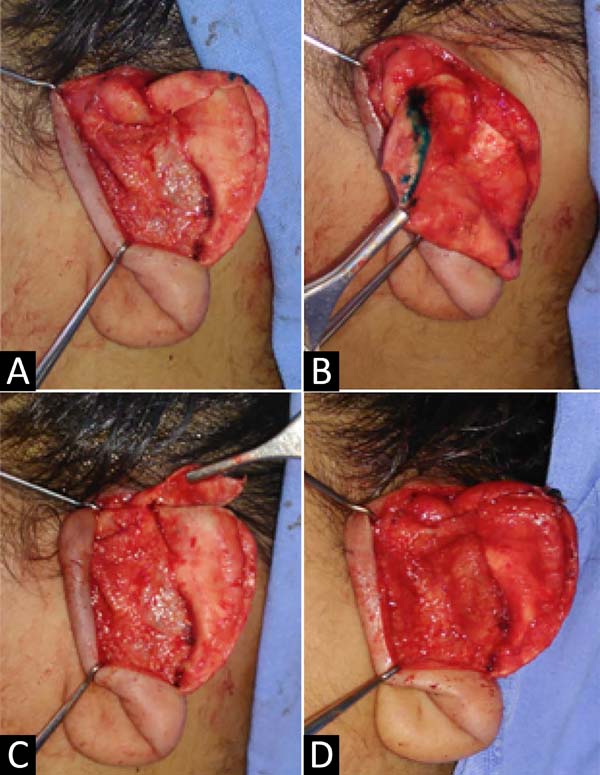
Retroauricular incision between the conchal cartilage and the helix in the lower and middle thirds and below the helix line in the upper third. The incision allows complete exposure of the auricular cartilage without excessive detachments.
Dissection in planes with complete helix, anti-helix, and scapula depletion exposing the cartilaginous alteration (Figure 2) completely.
Marking with methylene blue in the region of constricted cartilage. Incision in constricted cartilage along its entire length preserving 0.5 cm of the cartilage in the medial region. Then, we resected a small equilateral triangle of about 0.2 cm with an upper base to facilitate the posterior and inferior rotation of the cartilaginous flap (Figure 2).
Making U stitches with 5-0 nylon fixing a cartilage flap on the scapha, lengthening the outer ear in the craniocaudal direction.
Sewing of Mustardé stitches (1963)4 with nylon 4-0 in order to demarcate anti-helix and stitch in anti-tragus until the concha for lobe adduction (Figure 3).
At the end of the procedure, a dressing was applied with gauze soaked in neomycin sulfate solution, molding the shape of freshly made ear accidents and dry gauze and bandages covering them. The dressing was kept for 3 to 4 days without watering and in good condition.
An elastic restraint band with light compression was used during the first postoperative month. Photo-sun protection is indicated until complete healing.
Results can be seen 30 days after the operation and complete healing within six months of surgery (Figure 4).
DISCUSSION
Auricular deformities include a vast spectrum of deformities, ranging from pre-auricular appendages to the complete absence of the auricular pavilion. The set of alterations in the constricted ear is vast and of varying degrees of severity, ranging from mild defects, with changes in soft tissues, amenable to non-operative treatment, to moderate and severe defects that require surgical reconstructions1. Tanzer (1975)2 classified these degrees. Group I: helix collapse exclusively; group 2: deficiency of scapha, upper cross, and triangular fossa; group 3: intense constriction of the ear with fixation of the anterior helix close to the low lobe implantation of the ear. Different procedures have been described, these with varied results and reproducibility1-9.
At birth, up to 38% of babies have helical deformities; however, about 84% of them resolve spontaneously by the end of the first year of life. In mild cases, monitoring or using earmolds with immobilization of the ear can have reasonable results. If the deformity persists after the first year, the patient must be followed up, and surgical treatment instituted depending on the severity of the constriction10.
Given the wide variety of possible changes, the most important thing is to define whether there is the possibility of using local tissues or whether autologous cartilage and/or skin grafting is necessary11. Once the possibility of using local tissues has been defined, the cartilage flap proposed by Tanzer (1975)2 maintains the cartilaginous continuity and does not leave empty spaces, in addition to increasing the height of the ear, as evidenced in the reported case.
Although infrequent, the extrusion of nylon stitches used for cartilage reconstruction and Mustardé stitches (1963)4 is the main complication of this procedure12. Eventually, granulomas and even an infectious focus may form. The treatment consists of immediate removal of the streaked wires. This withdrawal will very rarely cause recurrence. Suboptimal relapse or treatment is the second most common complication, however, also with low incidence.
CONCLUSION
Auricular deformity in constriction is an uncommon malformation of the varied spectrum and challenging to manage. The described method is a versatile alternative for treating this disease; it can be used in a mild, moderate, and even severe spectrum of involvement, as long as there are local tissues that can be used for reconstruction.
REFERENCES
1. Elshahat A, Lashin R. Reconstruction of moderately constricted ears by combining V-Y advancement of helical root, conchal cartilage graft, and mastoid hitch. Eplasty. 2016 Jul;16:e19.
2. Tanzer RC. The constricted (cup and lop) ear. Plast Reconstr Surg. 1975 Abr;55(4):406-15.
3. Matsuo K, Hayashi R, Kiyono M, Hirose T, Netsu Y. Non-surgical correction of congenital auricular deformities. Clin Plast Surg. 1990;17:383-95.
4. Mustardé JC. The correction of prominent ear using simple mattress sutures. Br J Plast Surg. 1963 Abr;16:170-8.
5. Janz BA, Cole P, Hollier Junior LH, Stal S. Treatment of prominent and constricted ear anomalies. Plastic Reconstr Surg. 2009 Jul;124(1 Suppl 1):27e-37e.
6. Kaye BL, Lotuaco GG. A simplified technique for the correction of the congenital lop ear. Plast Reconstr Surg. 1974 Dez;54(6):667-70.
7. Musgrave RH. A variation on the correction of congenital lop ear. Plast Reconstr Surg. 1966 Mai;37(5):394-8.
8. Horlock N, Grobbelaar AO, Gault DT. 5-year series of constricted (lop and cup) ear corrections: development of the mastoid hitch as an adjunctive technique. Plast Reconstr Surg. 1998 Dec;102(7):2325-35;discussion:2333-5.
9. Stephenson KL. Correction of a lop ear type deformity. Plast Reconstr Surg. 1960;26:542-5.
10. Kelley P, Hollier L, Stal S. Otoplasty: evaluation, technique, and review. J Craniofac Surg. 2003 Set;14(5):643-53.
11. Franco D, Medeiros J, Andrade D, Grossi A, Franco T. Tratamento cirúrgico de orelhas constrictas. Rev Soc Bras Cir Plast. 2006;21(3):180-5.
12. Zanin EM, Maximiliano J, Oliveira ACP, Arpini NE, Duarte DW, Portinho CP, Collares MVM. Otoplasty: Rasps or Puncture Needles? A Clinical Trial. Aesthetic Plast Surg. 2020 Oct 29. doi: 10.1007/s00266-020-01972-z. Epub ahead of print. PMID: 33123781.
1. Hospital of Clinics in Porto Alegre, Porto Alegre, RS, Brazil.
EMZ Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Writing - Original Draft Preparation
ICS Analysis and/or data interpretation, Conceptualization, Data Curation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing
LVD Writing - Original Draft Preparation
CPP Supervision, Visualization, Writing - Review & Editing
ACPO Realization of operations and/or trials, Supervision, Visualization, Writing - Review & Editing
Corresponding author: Eduardo Madalosso Zanin, Rua Ramiro Barcelos, 2350, Rio Branco, Porto Alegre, RS, Brazil. Zip Code: 90035-007. E-mail: eduardo.zanin@gmail.com
Article received: July 12, 2019.
Article accepted: July 19, 2020.
Conflicts of interest: none









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter